California Universal Health Care Workbook - 2018
Committee Chair:
Timothy D. Bilash MD MS FACOG
Committee Member Contributors:
Philomena Lin MSW LCSW
George Phillips EE
John Kaplan MD FACOG
Marilyn R Lyons MPP JD Financial Sevices Representative
February 09, 2018
The Chair gratefully acknowledges the valuable participation through discussion, comment and writings over the past year; all involved have made significant contributions in shaping the Workbook. It is the product of over 1000 hours of Volunteer effort. I also am humbly indebted during this time for the continued dedication, love and acceptance of my dear Roya whose patience made this report possible. She displays the highest ethics and caring, bringing unbounded joy to every endeavor. I am very fortunate.
Responsibility for the accuracy and contents of the Workbook rests entirely with the Chair.
- California Universal Health Care Workbook - 2018
TABLE OF CONTENTS
I. California Universal Health Care Workbook Introduction - February 09, 2018
II. Health Delivery Principles to Consider
III. Health Insurance History
IV. ACO - Accountable Care Organization
V. The Collaborative Model (Non-Physicians as Physician Substitutes)
VI. The Managed Competition-Enthoven-Electronic Technologies/EHR conundrum
VII. Tax Policy, Economic and Business Policy Issues
VIII. Quality
IX. Cost
X. California State Single Payer Total Health Insurance (SB-562/SP2.3)
XI. California Single Payer (CSP2.3) Intents
XII. California State Single Payer (CSP2.3) Benefits
XIII. Single Payer / Other Health Systems - Exploring the State Health Insurance Cafeteria
XIV. Review of State Business Gross Receipts Taxes - Proposed funding mechanism in CSP/2.3
XV. Medicare Program Essentials - Retired Worker Health Insurance Program (1965)
XVI. Media Objections to SB-562 - Researching the Sources
XVII. Legislative Objections
XVIII. Evidence "Biased" Medicine - The "Big Medicine" Whitewash?
XIX. Electronic Technology
XX. Excess Profits
XXI. The application of Flawed Economic Theory to Medicine. Can we understand History?
XXII. Recommended Resources
XXIII. Recent Legislative Testimony to the Select Committee CA Assembly on SB-562 (February 5x, 2017)
back
back
-
Medical Insurance in the United States has a complex history, especially its
financial complexity
.
-
"Health insurance in the United States is a recent phenomenon, less than eighty years old.
Prior to the 1930s, employers, unions, and religious and fraternal groups occasionally offered health care or benefits to their members, but modern health insurance did not exist. Health insurance in its contemporary form can be traced to the hospital prepayment plan offered by Baylor
Hospital to the white public school teachers in Dallas, Texas in 1932."
( 148-05 ) 148-05 Microsoft Word - Jost GYMR.doc - The_Regulation_of_Private_Health_Insurance. pdf <<< OPEN - First implemented as a Payroll Tax (Partially deductable thru Employer).
- Led to the alternative Private Insurance (Cash) Volunteer Dependency, with Local Hospitals that increased Services
- Now State programs are subsidized by the Federal Government (Hill Burton, then Medicare/Medicaid since the 1960's)
- Experiences in other Countries/States may not helpful for cost issues, as Automation and Loss of the Middle Class are inevitable
-
Tying Health Care to Employment Payroll is flawed
, as 300 Million need care but only 100 million are working
-
"Health insurance in the United States is a recent phenomenon, less than eighty years old.
Prior to the 1930s, employers, unions, and religious and fraternal groups occasionally offered health care or benefits to their members, but modern health insurance did not exist. Health insurance in its contemporary form can be traced to the hospital prepayment plan offered by Baylor
Hospital to the white public school teachers in Dallas, Texas in 1932."
- Providing Access to Care
is an ill-defined concept:
- Health Care is really a Need
(often argued a Right versus Entitlement). Meeting that Need is the goal.
-
10 commandments of Healthcare ?
( 135-01 ) Craig M. Wax, DO Medscape August 19, 2017
"The Knots in Healthcare"
1. Health insurance is not healthcare.
2. Health insurance is not health.
3. Health insurance is not a right.
4. Healthcare is not a right.
5. Healthcare is not health.
6. Health is not a right.
7. Individuals are smartest and healthiest when self-motivated to do so by natural consequences.
8. No individual should be obligated to work for free or be extorted by federal government force majeure to purchase items or services for others.
9. Government regulations and third-party reimbursement increases costs and decreases efficiency.
10. Direct patient pay for free market competing services is most efficient, cost effective and promotes excellence.
TAGS - Visit or Procedure or Treatment as Available Care (promised
)
is not the same as Obtained Care (received
)
or Costed
Care (paid for
)
. Administratively and Politically, we conflate multiple parts of these process and give credit only to the Insurance coverages, leading to documentable Cost Shifting
and more recently Care Shifting
(especially in Hospitals).
- Libertarian views espouse that you should buy Care with your own money. Those who don't "work for it" don't deserve care. For the wealthy this is not an issue. Individual, Governmental and Corporate Investment Activities in Securities are considered the equivalent of work, rather than distribution of the pie created by economic goods and services produced. These investments however are taxed at lower rates than payroll.
SO WHAT IS THE ROLE OF GOVENMENT FOR SOMETHING EVERY PERSON NEEDS, BUT IN DIFFERING AMOUNTS? Maybe we can separate out the direct pay from the market competition part for examination. Agreement about the Public Commons is the Basis of Civilization, with consent of the Governed.
- Health Care is really a Need
(often argued a Right versus Entitlement). Meeting that Need is the goal.
-
Insurance and Administration of Medicine is extremely wasteful in the US
(
Estimated 1/3
of Annual Spending
)
-
Administrative Costs
for Health Care has Increased 3000%
in the U.S. from 1970-2009
171-02 growth of administrators.pdf <<< EXPAND GRAPHIC
-
Kaiser Family Foundation/Bureau of Labor Statistics
https:// me.me /i/3500-growth-of-physicians-and-administrators-1970-2009-3000-2500-2300-11964044
-
Kaiser Family Foundation/Bureau of Labor Statistics
-
Wasted Dollars
in US Health Care, 1/3 of $3 Trillion Dollars
, is well documented (2009). (
IOM
& Pollin
Analyses)
( 171-02 ) 171-02 IOM Report/ Estimated $750B Wasted Annually In Health Care System | Kaiser Health News.pdf
171-0 http://resources.nationalacademies.org/widgets/ vsrt / healthcare-waste.html ? keepThis =true& <<< VIDEO
-
171-01a excess health costs slide.pdf
<<< EXPAND GRAPHIC
-
171-01a excess health costs slide.pdf
<<< EXPAND GRAPHIC
-
Administrative Costs
for Health Care has Increased 3000%
in the U.S. from 1970-2009
-
Hospital Care increases Health Costs - the conundrum
. Hospitals are the most expensive place to give Medical Care. The US has continued to expand Hospital facilities, closing down smaller offices and moving them into larger consolidated Hospital-based facilities. They have taken on huge building programs and expansion of Hospital facilities
that now face budget shortfalls
. This has fueled an explosion in Administrative cost. It is the advanced stages of "
Vulture Capitalism
".
- Hospitals have always lost money on operations, requiring subsidy.
- The Hospitalist
/Collaborative Model introduces even more overhead
than prior systems.
- Hospitals have always lost money on operations, requiring subsidy.
-
US has astronomical Drug and Procedure Prices
.
-
US has fewer Physicians Per Capita
-
The US has fewer Physicians to care for patients than other countries.
177-07 Feb13_ Michener.pdf
177-07 per capita lower.pdf <<< EXPAND GRAPHIC
- 178-01 MDpercapitaGraphuc.pdf
<<< EXPAND GRAPHIC
-
The US has fewer Physicians to care for patients than other countries.
- Consumer attitude of Entitlement
is encouraged, without regard to resources accepting the broken system.
-
What needs are entitled, and Who deserves them? (dividing the pie, vs privileging from membership in a class; encourages tribalism)
- High School, College Education
- Food, Clothing, Shelter
- Medical Care
-
Cable Entertainment
-
THERE IS NO FREE LUNCH!
-
What needs are entitled, and Who deserves them? (dividing the pie, vs privileging from membership in a class; encourages tribalism)
back
back
- Insurance in the U.S.
- "Unlike other countries,
insurance regulation is conducted at the state level rather than at the national level in the U.S.
This has been the case since its inception and was reaffirmed by the Congress when it enacted the McCarran-Ferguson
Act (
MFA
) in 1945. The MFA
delegated the principal responsibility for regulating insurance to the states except in instances where the Congress chooses to intervene and establish federal authority over certain areas of insurance or firms involved in the business of insurance." (
148-01
) <<< OPEN
https://papers.ssrn.com/sol3/ papers.cfm ?abstract_id=2026898
- "At the Federal level, there are a number of important statutes applicable to health care insurance. The McCarran-Ferguson
Act provides that even though the insuring or provision of health care may be national in scope the regulation of insurance is left to the states. Likewise, the Health Maintenance Organization (HMO) Act
provides that HMO's or health service plans are regulated by the states....
in California health insurers are regulated by the Department of Insurance and HMO's and health service plans are regulated by the Department of Corporations
." (
148-08
) <<< OPEN
https://law.freeadvice.com/insurance_law/health_insurance/health_insurance_ regulation.htm
- "At its core,
the insurance relationship is based on a contract
under which the insured pays money to an insurance company at one point of time with the understanding that if certain losses described in the contract eventuate at a later point in time, the insurer will cover the loss. The insurer pools risk, collecting premiums from many insureds, only a few of whom will recover their full premium, at least in the short run (and many insureds have only a short-term relationship with health insurers.) The insurer, however, is at risk of paying out large sums of money for the benefit of a few of its insureds in the short run, and for the benefit of many more in the long run if the relationship persists. This relationship is inherently problematic.
" (
148-05
)
148-05 Microsoft Word - Jost GYMR.doc - The_Regulation_of_Private_Health_ Insurance.pdf <<< OPEN
- "First, its viability depends on the financial capacity of the insurer to respond to the claims of its insureds, the total of which can potentially exceed the sum total of premiums received."
- "Second, the insured depends on the insurer’s good faith and efficient business practices for the prompt and fair payment of claims. In the short run at least, it may be in the financial interest of the insurer to delay payment of claims and to dispute claims that are in any way questionable, or even to refuse to pay legitimate claims."
- "Third, an insurance contract is typically a long and complex instrument, drafted by the insurer . Few terms, if any, are negotiated. It is what is known in the law as an adhesion contract. The insured is largely dependent on the insurer for assuring that this contract meets the reasonable expectations of the insured as to the coverage that is being purchased and that it does not contain terms that can be used unfairly to deny coverage when risks eventuate. The insured is largely dependent on the insurer for assuring that this contract meets the reasonable expectations of the insured as to the coverage that is being purchased and that it does not contain terms that can be used unfairly to deny coverage when risks eventuate."
- "Finally, the insured is largely dependent on the marketing practices of the insurer to understand the nature of the insurance product that is being purchased and to avoid unreasonable expectations as to the extent of coverage."
- "
The insurance transaction is further complicated by the problems of adverse selection and moral hazard
.... An insured driver may drive less carefully, a person with health insurance may smoke more or exercise less.... The classic example of moral hazard is the insured ship owner scuttling a ship to collect on the insurance policy."
- "A number of arguments support giving the states more power to reform health insurance. The states are closer to, and thus more responsive to, the needs of their citizens
; states are freer to experiment
and thus to identify more varied and better solutions to problems than the monolithic federal government; states are better able to address regional variations in health care needs and preferences. Allowing states to take different approaches also allows persons or businesses with preferences for more or less health care coverage or expenditures a range of options. On the other hand, s
ignificant arguments can be made for health care reform at the federal leve
l
."
( 148-05 ) 148-05 Microsoft Word - Jost GYMR.doc - The_Regulation_of_Private_Health_ Insurance.pdf <<< OPEN
- The fundamental higher cost for private insurance
is obvious. "
Health insurance companies must make money to stay viable
. To make money, the insurance company sets premium rates according to risk. If the insurance company covers mostly healthy people, there is good chance money will be left over at the end of the day... [many] insurance regulators come from a previous life of being (drum roll here) – insurance industry executives... Or they work in regulation and may move to jobs in (another drum roll) – the insurance industry.
https://www.forbes.com/sites/ carolynmcclanahan /2012/06/19/should-states-really-regulate-health-insurance/#1f6c3b88b8bd ( 148-02 ) <<< OPEN
- "
Workers who buy individual health insurance policies
, in sharp contrast to workers enrolled in employer-based group insurance, do not enjoy the generous tax breaks that accompany the purchase of employer group plans
. Because non-group markets are a market of last resort for so many individuals, the cost of premiums in these markets likely affects whether or not many of these Americans can afford to purchase health insurance for themselves and their families."
http://www.healthinsuranceindepth.com/ individual-state-guides.html ( 148-07 ) <<< OPEN
- The State of Texas Website describes Health Insurance decisions facing patients, particularly for Plan Comparisons.
( 148-09 ) http://www.tdi.texas.gov/pubs/consumer/cb005.html#rates
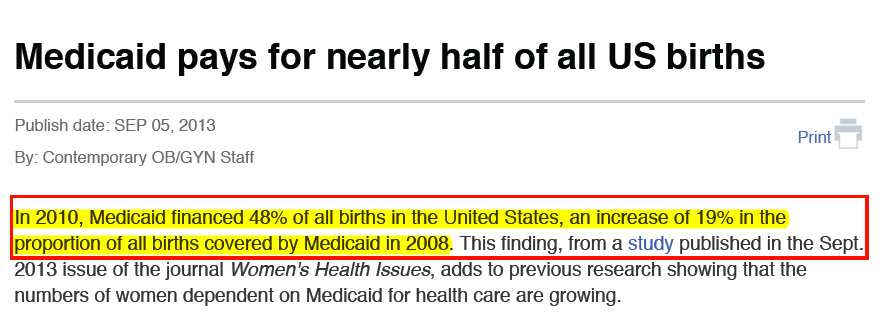
- Medicaid pays for nearly half of all US births.
(152-01) 152-01 Medicaid pays Contemporary OBGYN.pdf
- It is useful to remember that In-Office services were not covered by insurance until more recently
. Blue Cross/ Blue Shield Hospitalization policies were introduced, but they only covered a limited number of out-patient follow-up appointments. Office Care charges were paid as a commercial transaction (cash, on-time, or written off).
- "Unlike other countries,
insurance regulation is conducted at the state level rather than at the national level in the U.S.
This has been the case since its inception and was reaffirmed by the Congress when it enacted the McCarran-Ferguson
Act (
MFA
) in 1945. The MFA
delegated the principal responsibility for regulating insurance to the states except in instances where the Congress chooses to intervene and establish federal authority over certain areas of insurance or firms involved in the business of insurance." (
148-01
) <<< OPEN
- Insurance Regulation
- State Regulation of Health Insurance
- "In California, health insurance is regulated by the California Department of Insurance
(
CDI
)."
https://www.insurance.ca.gov/01-consumers/110-health/10-basics/ health-ins-reg.cfm ( 148-03 ) <<< OPEN- Reviews every policy for sale in California to make sure that it follows the law
- Offers consumer support about your policies, file a complaint, or contest a decision by your insurers;
- Investigates fraud and takes enforcement action when necessary
- Reviews insurance companies' finances to make sure that they are stable
- Licenses brokers and agents who sell insurance in California
- "In California, health insurance is regulated by the California Department of Insurance
(
CDI
)."
- Proposals to regulate Health Insurance at the Federal Level instead of the State Level (2005)
- "The Small Business Health Fairness Act of 2005 (
H.R
. 525), the Health Care Choice Act of 2005 (
H.R
. 2355), and H
ealth Insurance Marketplace Modernization and Affordability Act of 2005
(S. 1955) [had it been] enacted
would fundamentally change the way health insurance is regulated in the United States
. In this context, the future of health insurance regulation is not entirely clear." "The three bills intend[ed] to make markets more competitive by making it easier for insurance companies and associations to operate – not having to do business within the constraints of 51 different sets of regulators and rules.
( 148-12 ) https://www-tc.pbs.org/now/politics/ Healthinsurancereportfinalkofmanpollitz . pdf <<<OPEN
- An unintended consequence, however, may be to allow new ways to segregate health insurance markets by risk. Consequently, to the extent that current insurance regulations have reached a balance in promoting competition while ensuring an equitable spreading of risk – through rating, covered benefits, and other rules that protect access to coverage by healthy and sick alike – the segmented market could destabilize premiums and coverage.
Ironically, this may lead to a reduction in protection from medical expenses that health insurance offers individuals, families, and employers. It may lead to no private health insurance options for consumers with medical needs and fewer choices for others. It remains to be seen what direction for health insurance regulation the Congress may set, and what changes in private coverage may result."
"Congressional sponsors appear to depart from traditional reliance on states as laboratories for innovation and as primary regulators of health insurance. In the past, federal legislation established a floor of national standards. The three proposals would do the opposite . Also, while in the past Congress heavily relied on states to implement federal standards, the bills pending in Congress would substantially restrict state ability to regulate health insurance.
"All three bills would also have the effect of reducing the overall level of health insurance regulation by any level of government. While they would restrict authority of states to regulate risk selection, to limit unfair market practices, and to engage in oversight, none of the proposals would invest substantial new regulatory authority or capacity with the federal government. In this respect, the three bills could be viewed as de-regulating health insurance to varying degrees."
( 148-12 ) https://www-tc.pbs.org/now/politics/ Healthinsurancereportfinalkofmanpollitz . pdf <<< OPEN
- "Other federal laws also affect insurance coverage. Congress has adopted three coverage mandates, requiring insurance plans to provide forty-eight hours of hospitalization for a normal delivery and ninety-six hours for a Cesarean section, to pay for breast reconstruction if they cover mastectomies, and, subject to a number of exceptions, to not apply annual and life-time limits to mental health coverage that are less generous than those applied to physical health coverage.
The Age Discrimination in Employment Act requires employers in general to offer the same coverage or coverage of the same value to their employees regardless of age, while the Pregnancy Discrimination Act requires employee benefit programs to cover pregnancy and childbirth related services. The Americans with Disabilities Act (ADA) prohibits at least intentional discrimination against the disabled in insurance underwriting, although as a practical matter it permits insurers to take health status into account as long as they do so rationally."
https://www.nasi.org/ usr _doc/The_Regulation_of_Private_Health_Insurance . pdf ( 148-05 ) <<< OPEN
- "in the end, our experience with insurance and managed care reform would seem to teach us that it is very difficult to make private, for-profit, insurers behave as anything other than private for-profit insurers. The surest route to profit for an insurer is to attract the lowest risk applicants available at any given premium.
There is always more money to be made by an insurer by managing risk exposure than by trying to manage health care costs. Beyond this, insurers that intend to remain in the market try to provide as generous benefit packages as the market demands and to maintain a reputation for good service, at least to low-cost insureds.
Regulatory efforts may budge insurers slightly from these business strategies, but rarely much or for long. This is particularly true in the current environment, in which any insurer, employer, or individual can simply cease to sell or buy insurance if it does not like the opportunities or options available at any given moment in any given market. " ( 148-05 ) <<< OPEN
- "Of course, insurance can be made more affordable by allowing it to cover less. “
Barebones
,” high cost-sharing policies sold in the individual market to young, healthy individuals can be quite inexpensive. But these policies also leave those who purchase them exposed to considerable financial risk, as well as to the possibility of not being able to afford health care when it is needed
. A number of studies have been published in recent years examining the plight of “underinsured” Americans. Nearly one in six American families spent more than ten percent or more of their income (five percent or more if low income) on out-of-pocket medical costs in 2001–02
.
These families were more than twice as likely not to obtain needed medical care and half again as likely to delay or have difficulty finding needed care as insured Americans generally. Another study found that adults with health problems with deductibles above $500 (and particularly those with incomes below $35,000 a year) are much more likely than those with lower deductibles not to fill a prescription, not to get needed specialist care, to skip a recommended test or follow-up visit, or to have a medical problem for which they have not sought medical care.
Patients with high deductibles are also much more likely to have problems with medical bills or medical debt. Nearly half of “underinsured” adults were contacted by a collection agency about medical bills in the year before a recent survey, while more than one-third said that they had to change their lives significantly to pay for medical bills.... Nevertheless, many American households would be stretched were they required to bear the full cost of health insurance premiums out of pocket ."
https://www.nasi.org/ usr _doc/The_Regulation_of_Private_Health_Insurance . pdf ( 148-05 ) <<< OPEN
- "It should be noted that insurance costs in the individual market can have a large impact on the number of uninsured individuals. The individual market is effectively a residual market, consisting largely of those without access to employer-sponsored insurance
. Workers who buy individual health insurance policies, in sharp contrast to workers enrolled in employer-based group insurance, do not enjoy the generous tax breaks that accompany the purchase of employer group plans.
Because non-group markets are a market of last resort for so many individuals, the cost of premiums in these markets likely affects whether or not many of these Americans can afford to purchase health insurance for themselves and their families.... Furthermore, emerging economic trends will likely increase the share of the working population without access to employer-sponsored insurance."
Heritage Foundation Health Insurance Regulations State-by-State 2005
http://www.healthinsuranceindepth.com/ individual-state-guides.html ( 148-06 ) <<< OPEN
- "The Small Business Health Fairness Act of 2005 (
H.R
. 525), the Health Care Choice Act of 2005 (
H.R
. 2355), and H
ealth Insurance Marketplace Modernization and Affordability Act of 2005
(S. 1955) [had it been] enacted
would fundamentally change the way health insurance is regulated in the United States
. In this context, the future of health insurance regulation is not entirely clear." "The three bills intend[ed] to make markets more competitive by making it easier for insurance companies and associations to operate – not having to do business within the constraints of 51 different sets of regulators and rules.
- "Could the fact that
insurance regulators are significantly intertwined with the insurance industry explain the lack of protection for consumers in many states? Texas is a great example... many state insurance regulators come from a previous life of being (drum roll here) – insurance industry executives. Or they work in regulation and may move to jobs in (another drum roll) – the insurance industry. This also happens on the federal level." It looks like the Professional Physicians and Nurses have been shunned.
https://www.forbes.com/sites/ carolynmcclanahan /2012/06/19/should-states-really-regulate-health-insurance/#1f6c3b88b8bd ( 148-02 ) <<< OPEN
back
- State Regulation of Health Insurance
back
- "Developed nearly a decade ago to help rein in the growth of Medicare spending and improve patient outcomes, ACOs
now are gaining attention as a way for independent practices to lessen their reporting burden under Medicare’s new payment system while possibly increasing their revenue." (2017)
( 40-03 ) 40-03 Top risks and rewards of ACOs . pdf <<< OPEN
- "Depending on the type of ACO , membership could carry financial risk . It may also mean practices must adopt new information technology , as well as giving up some autonomy."
- "a major goal of the 2015 Medicare payment reform law was to move the program away from fee-for-service in favor of value-based reimbursement systems."
- “ We’re seeing a big ramp-up in [practice] consolidation , whether it’s through an ACO or something else, because [ MIPS ] is a heavy financial and workflow lift, and to get the necessary support as an independent provider is pretty tough ,” says Steffany Whiting, strategy and marketing officer with CHESS, a firm that provides management services to ACOs .
-
ACO's
offer Centralized Corporate Control, with vertical and horizontal integration, allowing a merger of tax and tax-exempt processes
.
- Why Accountable Care Organizations Are Like Vegan
Barbeque.
( 40-05 ) 40-05 Why accountable care organizations are like vegan barbecue . pdf <<< OPEN
The ACO system has been evolving in hopes of cost containment. Despite the advantage of expanded access to Primary Care, No pre-existing exclusions or Maximum Limits, there are consequences.
-
1 Jeff Goldsmith .
pdf
<<< Intro
- 2 ACO's
Hosp
marginalize doctors .
pdf
<<< Prediction on Costs
-
3 US halved specialist pay .
pdf
<<< Decreased Physician Reimbursement
-
4 judgement pay too low .
pdf
<<< Medical Judgement Excluded from Reimbursement
-
1 Jeff Goldsmith .
pdf
<<< Intro
- "CMS
has now conducted three demonstrations of the 'accountable care organization,' and all of them have failed
...The taxpayer has now financed three ACO
demonstrations – the PGP
, Pioneer, and MSSP
demos. (6/2017)
( 40-02 ) 40-02 Would ACOs Work If They Were Turned Into HMOs? THCB <<< OPEN
- Pioneer ACO
program
, which ran from 2012 through 2016, cut Medicare spending by three- or four-tenths of a percent on average over its first four years.
-
Physician Group Practice (
PGP
)
Demonstration, which ran from 2005 to 2010, raised Medicare costs by 1.2 percent.
-
Medicare Shared Savings Program (
MSSP
)
, which began in 2012 and may lumber on indefinitely, has raised Medicare costs by two-tenths of a percent on average over its first four years.
- "It is way past time for CMS
and health policy researchers to determine why all three ACO
demos failed
."
( 40-02 ) 40-02 Would ACOs Work If They Were Turned Into HMOs? THCB <<< OPEN
-
ACO
(and private insurance) in-Network requirements are a form of Partial-HMO. "M
any Medicare recipients in FFS
Medicare are there because they don’t want to enroll in a Medicare Advantage plan, and they’re hoping Medicare beneficiaries will be too dumb to notice that they’re being offered a bribe to enroll in an HMO dressed up as an ACO
... Once you comprehend how confused the doctors are, you’ll shake your head and wonder how anyone could think patients will ever understand the flabby ACO
concept.
- Although ACO
proponents claimed ACOs
would be “run by doctors” and would therefore be kinder and gentler than HMOs, it turns out doctors not only didn’t run the Pioneer ACOs
, they had a poor understanding of what their ACOs
were doing to and for them. According to L&M’s final evaluation of the Pioneer program, “The vast majority of providers participating in Pioneer ACOs
were not directly part of the decision to participate, but rather were employed by or part of a medical group that joined the ACO
... The one feature of ACOs
the great majority of doctors understood clearly was that ACOs
impose more paperwork on doctors. “Approximately three-quarters of Pioneer physicians indicated that participation had required them to increase time spent on administrative, documentation, and reporting tasks…”
- “Representatives from many of the Pioneer ACOs
noted that
it was more difficult than initially anticipated to manage beneficiary utilization and patient visits outside of the ACO
."
-
ACO
managed care methods, "
guarantees high churn rates among doctors and patients
, shunts sicker patients away from the ACOs
, and assigns few ACO
patients to each ACO
doctor...
Evidence-free decisions
led to CMS’s
plurality-of-visits method
."
-
ACO
(and private insurance) in-Network requirements are a form of Partial-HMO. "M
any Medicare recipients in FFS
Medicare are there because they don’t want to enroll in a Medicare Advantage plan, and they’re hoping Medicare beneficiaries will be too dumb to notice that they’re being offered a bribe to enroll in an HMO dressed up as an ACO
... Once you comprehend how confused the doctors are, you’ll shake your head and wonder how anyone could think patients will ever understand the flabby ACO
concept.
- "It is possible that some of the managed care tools ACOs
are expected to use... (would at least improve quality and might lower costs as well) if they were applied to subsets of the chronically ill
." "
It’s clear those tools are never going to work if they are applied to entire 'populations.'
Managed care proponents must stop thinking in terms of structures (
ACOs
, HMOs, 'integrated systems,' 'medical homes') that apply managed care magic to entire populations, and start thinking in terms of specific services delivered to subsets of the chronically ill
."
-
Could we move to the Specialist as the primary care provider for these ill individuals rather than gate-keepers?
-
Could we move to the Specialist as the primary care provider for these ill individuals rather than gate-keepers?
- Measuring ACO
performance
-
(40-06) 40-06 ncqa
_
aco
_measures_fact_sheet_0 .
pdf
<<< OPEN
-
"
NCQA
now has the performance measures that Accountable Care Organizations (
ACO
) need to deliver better quality care at lower costs
. ACOs
coordinate doctors, hospitals and other health professionals to make sure people get all the care they need, while fighting waste and overuse. This requires collecting, integrating and using data to provide high quality, well-coordinated, patient-centered care and identify where ACOs
can improve quality and efficiency
."
-
"
NCQA
now has the performance measures that Accountable Care Organizations (
ACO
) need to deliver better quality care at lower costs
. ACOs
coordinate doctors, hospitals and other health professionals to make sure people get all the care they need, while fighting waste and overuse. This requires collecting, integrating and using data to provide high quality, well-coordinated, patient-centered care and identify where ACOs
can improve quality and efficiency
."
-
(40-06) 40-06 ncqa
_
aco
_measures_fact_sheet_0 .
pdf
<<< OPEN
- Pioneer ACO
program
, which ran from 2012 through 2016, cut Medicare spending by three- or four-tenths of a percent on average over its first four years.
- "New Generation" ACO
- adding more downside risk to offset increased cost?
( 40-04a ) 40-04a ACOs Plan to Move to Downside Financial Risk, Capitation Contracts . pdf (2017) <<< OPEN
- History of next generation ACO
Types -
There has been a constant flux in care models even since ACO's have been introduced, each change initiated when the last failed to meet its promise. The NeXt Gen ACO Model is "similar to the Pioneer Model but with higher potential rewards and risk than MSSP Tracks. Next Gen aims to transition providers from fee-for-service to capitation."
( 40-03 ) 40-03a ACO Types Compared . pdf <<< EXPAND
-
"
ACOs
anticipate entering downside financial risk contracts within the 10 months for shared savings/losses arrangements and 17 months for capitation, a survey showed." "Organizations across payers are also bearing similar financial risk levels. About 53 percent of ACOs
said that their organization has the same financial risk levels in their commercial and Medicaid contracts as their Medicare arrangements."
- "Only 28 percent of physician-led ACOs
have an active risk-based contract, whereas almost one-half (48 percent) of hospital-led ACOs
are assuming downside financial risk."
-
"
With ACOs
spending a significant portion of their budgets on health IT and care management, organization leaders are finding cost reductions to be a major challenge
.
"
- "Most ACOs
offer services for primary care (94 percent), labs and imaging (77 percent), specialty care (74 percent), and inpatient care (71 percent). Only
7 percent offer dental care
, 39 percent have long-term care
, and 49 percent manage pharmacy services
." Note that SB-562(CSP2.3) is wet to cover Dental, Long-term Care, and negotiate Pharmacy over-costs down.
-
Southern California had long relied on the Administrative contributions by the Independent Physician Practices, and is late to the transformation into Managed Care Models. Not much public attention is being paid to these problems. History repeats itself, with a twist.
(Please see
40-02
40-02 Would ACOs
Work if They Were Turned into HMOs? | THCB.pdf
)
-
Patient Centered Care
- decentralize the centralization under a coalesced corporate control
- Organizations are bought up, the administrative financial control retained, remainder allowed to atrophy.
- Caregivers deliver patient-centered care in an open environment that provides access to systematic analysis of all available evidence in electronic format from an extensive, ever-changing, continually updating, reliable statistical set. (011896)
-
Mimics arbitrage activity of financial merger and sell-off, as if the mission of the organization is organizing.
- History of next generation ACO
Types -
-
Downside Risk
(I keep the profit, You take the loss)
- One of the differences between now and the Hospital Financial Crash in the late 1990's is who was liable for the losses
. At that time Hospital Systems had moved into Capitation/Managed Care Models, and had bought up Private Practices in an effort to further the desired consolidation. Attending Physicians sold their practices to the Hospital Systems, and continued on as Employees. The worked in the same office as before. They used the same Staff as before. The saw the same patients as before. They were just owned on paper by the Hospital.
- Only problem was, Hospitals went broke
doing this. They had to be bailed out of the financial mess. In particular, the Federal Government took on a huge debt (still not paid off) to infuse cash into the Hospitals. They sold off the Practices, and bought out the Doctors' contracts. The Big Managed Care retreated, and many things went back towards the former systems. The Hospitals lost. The Doctors mostly retired early with a great nest egg and moved down to Florida.
- In the current setting, Physicians and Employees particularly take on "downside risk"
and are responsible as investors in the ACO
Corporations. As the crisis in other Industries, pension funds and retirement health funding become at risk as assets of the Corporation. Health Care Corporations are again facing huge loses and layoffs across the country to fill the financial gap: Banner Health Corporation laid off hundreds of workers nationwide including Physicians.
-
Medicaid has a habit of auditing an agency many years later - a Case in point is the San Diego Hospice, which had to declare bankruptcy and were sold off to Scripps Hospital. The well reported audit indicated they had been paid some tens of millions of dollars too much. Whether or not there were merits to the actions, the issue becomes who pays back the money. New, essentially deferred debt suddenly becomes due, having exaggerated benefit in the previous years.
San Diego Hospice could have been saved - San Diego news from inewsource
San Diego Hospice: The end of a journey
- The ACO
system as part of the Affordable Care Act (
ACA
) is problematic in this regard, because there is increased Risk assumed by this approach and increased Administrative Overhead to mine any savings.
-
Scripps Health (San Diego)
fired their CEO and are dealing with a
$30 Million dollar budget gap this year
.
- 2015 - Scripps dedicates $500 Million to EPIC computer system.
(40-11) 40-11 Physician 40-11 News Stories September 2015. pdf <<< OPEN
-
2017 -
"Scripps nixes hospital CEO positions and $30M in services"
( 40-12 ) 40-12 Scripps nixes hospital CEO positions and $30M in services _ Healthcare Dive . pdf <<< OPEN
"Scripps Health is cutting hospital C-suite positions and slashing $30 million from corporate services in an effort to remain viable in today’s changing healthcare environment, Modern Healthcare reported."
- 2015 - Scripps dedicates $500 Million to EPIC computer system.
-
The Sharp Health System (San Diego)
abandoned the Pioneer Managed Care program.
-
2012
- Sharp's Pioneering ACO
May Raise Bar in San Diego
(
40-08
)
- "One thing at least some of the organizations are excited about is that eventually CMS would be willing to go to a capitated approach. I think a lot of these Pioneer ACOs , given that they are leaders in care coordination already, like that option," said John Pickering, principal consulting actuary with the actuarial and consulting firm Milliman ."
- "Pioneer ACOs are likely to find their infrastructure somewhat lacking, particularly as they take on functions historically performed by health plans.... Some of the things that they're going to need in place in order to be successful are utilization management functions, such as disease management, complex case management, preauthorization services, specialty referral management, and other analytic tools. In particular, financial and actuarial modeling, which has typically been performed at the health plan level, will be an important contributor to the success of these organizations"
- "Perhaps the biggest challenge Pioneer ACOs
will face is that beneficiaries have the freedom to visit any health care provider accepting Medicare and not stay within their assigned ACO
network."
-
2014
-
"Sharp HealthCare
ACO
drops out of Medicare's Pioneer program"
( 40-10 ) Sharp HealthCare ACO drops out of Medicare's Pioneer program - Modern Healthcare . pdf <<< OPEN
- "Another Medicare Pioneer accountable care organization has exited the program, renewing questions about its long-term sustainability. Sharp HealthCare
, a five-hospital system in San Diego, said... that it dropped out of the Pioneer ACO
program."
- "Another Medicare Pioneer accountable care organization has exited the program, renewing questions about its long-term sustainability. Sharp HealthCare
, a five-hospital system in San Diego, said... that it dropped out of the Pioneer ACO
program."
-
2012
- Sharp's Pioneering ACO
May Raise Bar in San Diego
(
40-08
)
-
Scripps Health (San Diego)
fired their CEO and are dealing with a
$30 Million dollar budget gap this year
.
- One can think of the money problem using an analogy. When investing in Certificate of Deposit or Savings Bond, there is a guaranteed payout amount. The principle can not be lost. The purchase of stock has a downside risk - potentially the entire value of the stock can be lost. This is what ACO's
are moving into. An additional type of risk is the equivalent of buying on margin, when you potentially owe more than than was invested; Hospital Administration as Stock Option Trading. This is where we are.
- One of the differences between now and the Hospital Financial Crash in the late 1990's is who was liable for the losses
. At that time Hospital Systems had moved into Capitation/Managed Care Models, and had bought up Private Practices in an effort to further the desired consolidation. Attending Physicians sold their practices to the Hospital Systems, and continued on as Employees. The worked in the same office as before. They used the same Staff as before. The saw the same patients as before. They were just owned on paper by the Hospital.
- Comparing ACO
(Accountable Care Organizations) to FFS
(Fee-For-Service) Performance
-
A comparison of
fee-for-service to ACO's
indicates cost saving in some cases
. However, when results are scrutinized in one of the reports as an example, FFS
patients were 2 years older in the first years, and mortality was actually 6% better in the FFS
group than ACO
in the later years, skewing results.
( 40-18 ) ACOvsFFS joi150049 . pdf <<< OPEN
ACO vs FFS . pdf <<< EXPAND
-
A comparison of
fee-for-service to ACO's
indicates cost saving in some cases
. However, when results are scrutinized in one of the reports as an example, FFS
patients were 2 years older in the first years, and mortality was actually 6% better in the FFS
group than ACO
in the later years, skewing results.
-
Accountable Care Organizations in California
https://bcht.berkeley.edu/sites/default/files/ accountable-care-orgs-in-ca . pdf ( 158-0 ) <<< OPEN
-
Aggregation of Medical Groups across Regions has been unsuccessful.
Rapid Expansion through Mergers and Acquisitions can increase market stability, but Economies of Scale have not materialized
.
1Healthcare is local, 1990's . pdf <<< EXPAND
-
ACO
Utilization Cost Advantage has diminished.
3ACO less cost advantage . pdf <<< EXPAND
-
Capitation requires Non-Uniform Payment Mechanisms.
2Capitation, farm subsidies, malpractice burden . pdf <<< EXPAND
-
Size: Economies and Diseconomies of Scale
4More admin, no economies of scale . pdf <<< EXPAND
-
HMOs require Regulation which Increases Cost
5HMO failure . pdf <<< EXPAND
-
ACOs
are not a Panacea for Health Care Spending Control
7short term evaluations . pdf <<< EXPAND
-
Aggregation of Medical Groups across Regions has been unsuccessful.
Rapid Expansion through Mergers and Acquisitions can increase market stability, but Economies of Scale have not materialized
.
- Delivery Care Complexity and the Development of ACOs
.
1-
InTheBeginning
.
pdf
<<< EXPAND
-
In the Beginning Patients needed care, and paid when they could.
-
Then Hospitals were needed.
2-
ThenHospitals
.
pdf
<<< EXPAND
-
Hospitals were increasingly expensive.
3-
HelpWithTheBills
.
pdf
<<< EXPAND
-
Keep the Costs down with Administrative oversight.
4-
ManagedCare
.
pdf
<<< EXPAND
-
Cover the uninsured retirees.
5-Medicare .
pdf
<<< EXPAND
- Creation of ACO's
.
6-
ACOs
.
pdf
<<< EXPAND
- The Future? ACO's
using Certificated Providers.
7-
ACOsplusCertified
.
pdf
<<< EXPAND
-
Structural Issue Complexity in the Affordable Care Act (Scripps Summit 2016)
Hope and Reality - There is No Administrative Visibility of Physicians and Nurses
ACO Chart (no md or pts ) . pdf <<< EXPAND
-
In the Beginning Patients needed care, and paid when they could.
back
back
- The Rise and Falls of Physician Trained Authority
- Medicine in the American Colonial Period
- During the colonial and early federal periods (the height of "heroic medicine"), purgings
, bleedings, and high doses of toxic drugs constituted treatment for almost every condition. The public developed a very skeptical attitude towards regular doctors. Bands of "Sects" freely gave medical advice, emphasizing the participation of the patient in his or her own treatment.
- Perhaps over-promising and use of marginal treatments has awakened a tremendous mistrust of Medicine once again and the trust in Internet "do-it-yourself" medicine. It makes us more vulnerable to fads and "quack medicine", which at one time had even been legal in London. Slowly, scientific understanding replaces these practices but it has become difficult to bridge the knowledge-gap.
( 106-01 ) Bankrupt Hospitals in England Turn to Private Sector | Managed Care magazine
- During the colonial and early federal periods (the height of "heroic medicine"), purgings
, bleedings, and high doses of toxic drugs constituted treatment for almost every condition. The public developed a very skeptical attitude towards regular doctors. Bands of "Sects" freely gave medical advice, emphasizing the participation of the patient in his or her own treatment.
- Increasing surveillance of Physicians in Current Times
- A requirement took effect in January 2008, requiring hospitals to establish a “Focused Professional Practice Evaluation” for physicians, such as a sentinel event, a near-miss, complaints from staff or patients, or not meeting benchmarks during the ongoing evaluation process. We have entered another period of distrust.
141-01 ACOG Today, January 2008 - acogToday0108 . pdf ( 141.01 )
- There are few provisions for evaluating CEO and Administrative Staff malfeasance, except through the Hospital System Boards (
ie
, shareholders). CEO's convicted of child abuse and sexual abuse (which can include worker abuse) have gone undetected for years in too many cases.
- A requirement took effect in January 2008, requiring hospitals to establish a “Focused Professional Practice Evaluation” for physicians, such as a sentinel event, a near-miss, complaints from staff or patients, or not meeting benchmarks during the ongoing evaluation process. We have entered another period of distrust.
- Medicine in the American Colonial Period
- The "Collaborative Model" in Medicine promotes the Non-Physician as a Clinician, Administrator and Executive
. It has evolved from the original role functioning as "Physician Extender"; to actually replacing Physicians both in Primary Care and Specialties. It has been continuously supported by Medical Organizations like the American Medical Association (AMA) and the American College of Obstetricians and Gynecologists (
ACOG
).
- Evolution of the Model
- The "Collaborative Model" is based on an Academic Theoretical framework, pursued for over 50 years by the Institute of Medicine (
IOM
).
- It deconstructs patient care into smaller more similar tasks requiring less training, much as car repair in a body shop would operate. People get categorized as to their common, interchangeable illnesses that make factory care more efficient. However, the expectations require performance beyond their training level, seen as "efficient".
- Who is Primary Care - Provider Class Ambiguity
- MA, PA-C, NP, RN, MD, Specialist, Sub-Specialis , CRNA , CCA , CHPE ... titles are examples. (145-01)
- Medicine versus Nursing vs Technical vs Clerical
- Practitioner Title Inflation and the loss of the Medical Middle Class
- Swap Titles of Nobility for Professional Accomplishment
- Swap Titles of Nobility for Professional Accomplishment
- The "Collaborative Model" is based on an Academic Theoretical framework, pursued for over 50 years by the Institute of Medicine (
IOM
).
- Diagramming the Collaborative Model
( 144-02 ) 144-02 collaborativemodelgraph.pdf
- Administrative View of the Collaborative Model
175-02a Triple Aim Scripps Quality Summit Syllabus 2013. pdf
- Where are the Doctors and Nurses?
- Where are the Doctors and Nurses?
- How Nurse Practitioners Obtained Provider Status
(40-20) How Nurse Practitioners Obtained Provider Status pdf <<< OPEN
- Brief Timeline of the Collaborative Model in Maternity Care (The ACOG-ACNM
Project)
(133-0) 133-0 Essential Components of Successful Collaborative Maternity Care Models . pdf <<< OPEN
- [1971]
High-quality maternity care could be provided by teams
of Physicians, Nurse-midwives, Obstetric nurses, and others. These teams would be directed by a "qualified Obstetrician-Gynecologist"
[
ACOG
Joint Statement on Maternity Care]
- [1972]
Academic health centers should educate health professions students together
, and other educational institutions should affiliate with interdisciplinary education programs [
IOM
Report] ("Committee Medicine")
- [1975]
"Obstetrician team direction" no longer means being physically
present [
ACOG
Supplemental Statement Guidelines]
- Responsibility for team care is accepted by the obstetrician-gynecologist. Compensation shifts from performance of activity to increased liability, and eventually to inadequate compensation.
- Arrangements for formal consultation with an obstetrician-gynecologist required, if team leadership is provided by a physician not trained in obstetrics and gynecology.
- A written agreement
is needed to clarify consultation and referral policies (may involve financial arrangements).
- [2001]
Removed the language for direction of the Maternity team by an Obstetrician
. Instead required inclusion of an Obstetrician with hospital privileges "on the team" to guarantee complete care
. [
ACOG
Revised Joint Statement]
- [2001]
Identified the need to redesign the way health professionals are trained
[
IOM
].
- [2010]
Nurses should be full partners
, with physicians and other health care professionals, to redesign health care in the United States [
IOM
]. The term reengineering was used in the 1990's for a similar process that flattened professional distinctions.
- [2011]
Collaborative Practice Review by American College of Obstetricians and Gynecologists and American College of Nurse Midwives.
- A general, an inductive approach
to qualitative content analysis
was urged based on statistical outcomes
and regimentation (Nurse approach).
- Note that the elimination of deductive methods implies the elimination of Science. Inductive methods may be utilized in Science, but sole reliance on them leads to well characterized statistical errors (for instance, using a confirmatory test for screening. Individual differences become subservient to global protocols.
- Physicians however are required to abide by randomized controlled trials and committee opinions offered by the Academic and Certfied Community.
- Most practices studies were based in urban areas and were part of larger teaching hospitals , limiting general validity.
- Practices utilize advanced practice nurse specialists
and sub-specialty physicians
from areas such as Neonatology, Perinatology
, Reproductive Endocrinology, Maternal-Fetal Medicine, Urogynecology
, and Gynecologic Oncology to enforce Opinions and Protocols.
- A general, an inductive approach
to qualitative content analysis
was urged based on statistical outcomes
and regimentation (Nurse approach).
- [1971]
High-quality maternity care could be provided by teams
of Physicians, Nurse-midwives, Obstetric nurses, and others. These teams would be directed by a "qualified Obstetrician-Gynecologist"
[
ACOG
Joint Statement on Maternity Care]
- Concerns about outcomes
under the Collaborative Model?
- US Perinatal
Mortality is worsening
(2% increase in California 2016)
- US Maternal deaths have increased
(doubled in California) with the initiation of the Collaborative Model
- "American women are more than three times as likely as Canadian women to die in the maternal period.
...in the U.S., maternal deaths increased from 2000 to 2014. Nearly 60 percent of such deaths are deemed preventable.
...In every other wealthy country, and many less affluent ones, maternal mortality rates have been falling "- 5/12/2017 What's Behind America's Maternal Death Rate
(182-03) 182-03 What's Behind America's Maternal Death Rate_ _ NPR.pdf
- 5/12/2017 What's Behind America's Maternal Death Rate
- "American women are more than three times as likely as Canadian women to die in the maternal period.
- Managed Care and Mid-Level Model has
failed to control costs
- "Employing nurse practitioners to provide first-line care in UK general practice is likely to cost the same or slightly more than employing doctors ."
- Costs are pushed off to the future , deflected or ignored. The emphasis is on Investment Profit.
- The Hospitalist
/
Laborist
Model is also
more costly
($200,000 per hospitalist
per year).
- Cost-effectiveness of Collaborative Telemedicine
for Depressive Disorders is uncertain
.
- Patients with disability for PTSD
(Post Traumatic Stress Discorder
) were randomly assigned to Telemedicine
Outreach for PTSD
(TOP)
or usual care. Only minor improvements in Quality of Well--?Being (
QWB
) and
quality-adjusted life years (
QALYs
) were found. The TOP intervention was relatively expensive
,
with costs totaling $2,029 per patient per year. Intervention costs were not offset by reductions in health care utilization costs, resulting in an incremental cost-effectiveness ratio of $185,565 per QALY
(
interquartile
range $57,675 to $395,743).
- ...There remains considerable uncertainty due to inconsistent results among included studies. Reviewed cost-effectiveness analyses differed considerably in terms of economic quality, and risk of bias remained uncertain in the majority of studies, due to insufficient reporting ...studies should be conducted in large and representative patient samples from a societal perspective, taking into account indirect costs."
- May 19, 2015 Cost-Effectiveness of Collaborative Care for the Treatment of Depressive Disorders in Primary Care: A Systematic Review (9-0)
- July 7, 2017 Cost-Effectiveness of Telemedicine-Based Collaborative Care for Posttraumatic Stress Disorder. ( 7-0 )
- Costs of Telemedicine-Based
Collaborative Care for Posttraumatic Stress Disorder were not offset by reductions in utilization costs
. In fact, no demonstrated cost savings are evident (
British Journal of General Practice July 2006)
- Patients with disability for PTSD
(Post Traumatic Stress Discorder
) were randomly assigned to Telemedicine
Outreach for PTSD
(TOP)
or usual care. Only minor improvements in Quality of Well--?Being (
QWB
) and
quality-adjusted life years (
QALYs
) were found. The TOP intervention was relatively expensive
,
with costs totaling $2,029 per patient per year. Intervention costs were not offset by reductions in health care utilization costs, resulting in an incremental cost-effectiveness ratio of $185,565 per QALY
(
interquartile
range $57,675 to $395,743).
- Study biases are apparent
and there is varying accounting for indirect costs. Assumes for example than Certified Nurse Midwives (
CNM
) are "known to be cost-effective providers with documented success". Comparisons need to be done based on equal-dollar funding
for system as well as outcome measures.
- Medical Care by Assistants and Nurses is arguably a Third World Model, compensating for limited Physician workforce.
- Ezekiel Emmanuel MD
has been one of the major National Proponents of the Collaborative Model
- Emmanuel originally proposed "universal health care could be guaranteed by replacing employer paid health care insurance, Medicaid, and Medicare with [government] health care vouchers
funded by a value-added tax." This is a regressive Tax, leaving individuals to negotiate charges for themself
. It is a free market approach championed in Economics by Milton Friedman.
- "You're going to free up doctors of paperwork
and a lot of stuff that could be done by other people
to focus on really important cases and the complex ones that don't fit right in the box... Physician assistants and registered nurses will play a greater role in treating routine illnesses, giving doctors more time to focus on "really important cases,.. We're going to shift what doctors do to the high end, where they are really valuable."
- Shifts the reward from what a person does to what "cost-effective" profit they generate ("hi-end")
- Shifts the reward from what a person does to what "cost-effective" profit they generate ("hi-end")
- Ezekial
Emmanuel expresses his view of the "physican extender" as a "physician replacer".
(4-0) Ezekiel Emanuel Reinventing American Health Care (2014)
Interview: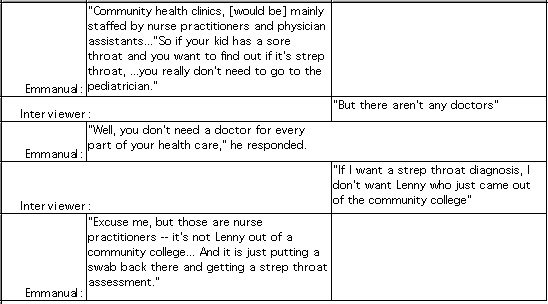
- Zeke
Emmanuel, Healthcare, Guaranteed
- (2-01) Pepperdine
Conference Video - March 23, 2017
Future of Health Care Symposium, Dr. Ezekiel Emanuel Remarks- "The Collaborative Model is a total failure."
- "The Collaborative Model is a total failure."
- Emmanuel originally proposed "universal health care could be guaranteed by replacing employer paid health care insurance, Medicaid, and Medicare with [government] health care vouchers
funded by a value-added tax." This is a regressive Tax, leaving individuals to negotiate charges for themself
. It is a free market approach championed in Economics by Milton Friedman.
- US Perinatal
Mortality is worsening
(2% increase in California 2016)
- Evolution of the Model
- "Purging" of the Medical Middle Class
- Non-Physician vs Physician Medical Care
(40-01) Are Nurse Practitioners Practicing Medicine
- In North Carolina, an NP (Nurse practitioner) is defined as a currently licensed registered nurse approved to perform medical acts
consistent with the nurse's area of NP academic
educational preparation and national certification
under an agreement with a licensed physician for ongoing supervision, consultation, collaboration, and evaluation of medical acts performed. This replaces the traditional view that doctors and nurses are trained and certified to practice in clinical programs.
- A removal of Clinical training in programs, replaced with Certificated Authority.
- In North Carolina, an NP (Nurse practitioner) is defined as a currently licensed registered nurse approved to perform medical acts
consistent with the nurse's area of NP academic
educational preparation and national certification
under an agreement with a licensed physician for ongoing supervision, consultation, collaboration, and evaluation of medical acts performed. This replaces the traditional view that doctors and nurses are trained and certified to practice in clinical programs.
- Degree Creep
- adding additional layers of certifications for higher paid, while lower paid levels have lower requirements.
- Academic Creep
- "Rising by degrees" is the term. Management titles, more required "diplomas" lead to higher salaries for physicians, survey shows, Michael Romano
( 143-01 ) December 2003, Modern healthcare 33(46):16.
143-01 rising by degree.pdf <<< OPEN
- "Like almost everyone else in the nation's increasingly sophisticated workforce, doctors who have the longest string of degrees or titles after their name tend to earn the highest salaries. And the more letters the better... Physicians in top management positions who have a master's degree in business administration in addition to their medical school diploma earn almost 35% higher salaries..."
- As well, Cejka
Search President Carol Westfall
indicates, "the key to success in healthcare-along with riches-continues to be day-to-day, hands-on experience as a manager.
- "Like almost everyone else in the nation's increasingly sophisticated workforce, doctors who have the longest string of degrees or titles after their name tend to earn the highest salaries. And the more letters the better... Physicians in top management positions who have a master's degree in business administration in addition to their medical school diploma earn almost 35% higher salaries..."
- "Rising by degrees" is the term. Management titles, more required "diplomas" lead to higher salaries for physicians, survey shows, Michael Romano
- Certification Creep
- A model study advocating providing MAs
for NPs
indicated that this would make NP utilization cost effective, implying that using NP's alone currently is not
cost effective. On the basis of the model parameters we use, the average cost of serving a patient can be reduced by ~10% if MAs
are hired to support NP
s
. It is a name that tunes approach.
- As well, their model assumed that MA's could be shared
. In practice this is not realistic because of issues of chaperoning, room turnover and patient education. Also, MA's are certificated workers, not academically or clinically trained in the traditional sense and can only provide very superficial interactions with patients. These models assume no RN involvement in care. Theoretical Models are commonly used to justify staffing decisions in Nursing, but apparently Physician medical judgements informed by Academics and Theory are not allowed in clinical care decisions.
- A model study advocating providing MAs
for NPs
indicated that this would make NP utilization cost effective, implying that using NP's alone currently is not
cost effective. On the basis of the model parameters we use, the average cost of serving a patient can be reduced by ~10% if MAs
are hired to support NP
s
. It is a name that tunes approach.
- Academic Creep
- Administrative excesses at Academic Centers
- Administrative problems at the University of California System is an example of widespread corruption problems:
- The Los Angeles Times wrote, "
UC
is far too inclined to use public money as a slush fund... UC
administrators have a disquieting tendency to run a loose ship, and run it by their own, rather than state or university rules. "improving the statistics became the mission of the program... UCI
Medical Center CEO Dr Ralph Cygan
"provided false information to keep the unit running."
- "
UC
leaders were recompensed, with as little public notification as possible; and about just how badly UCI
was mismanaged, despite the excellent compensation of its leaders..."
- "the UC cases suggest that lavish executive pay and perks at health care organizations, rather than being necessary to attract good leaders, actually correlates with bad leadership. Perhaps executives who are most concerned about their personal financial advancement are less likely to be devoted to the academic and health care mission."
- “University of California administration is paying excessive salaries and mishandling funds, state audit.... The audit of the UC
Office of the President appears to have uncovered the same kind of budgetary misrepresentations and executive excess that we’ve seen before with the State Parks Department and the Public Utilities Commission,” Rendon
said in a statement.
- More Trouble in the OC
: Golden Parachutes for UC
Leaders, and "Malfeasance" at UCI
,
( 143-02 ) 143-02 Health Care Renewal_ Search results for malfeasance at UCI . pdf 2005 <<<OPEN
- The Los Angeles Times wrote, "
UC
is far too inclined to use public money as a slush fund... UC
administrators have a disquieting tendency to run a loose ship, and run it by their own, rather than state or university rules. "improving the statistics became the mission of the program... UCI
Medical Center CEO Dr Ralph Cygan
"provided false information to keep the unit running."
- Administrative problems at the University of California System is an example of widespread corruption problems:
- Non-Physician vs Physician Medical Care
back
back
- Origins of Managed Competition
-
Alain Enthoven
, protege of Robert McNamara
(Ford Motor Company)
- Understanding driving forces behind this scheme and how it has left Medicine in rubble;
"Managed Competition" in Autos, War, Education and Medicine (has not worked).
- "
The phrase 'managed competition'
actually came from [Robert] McNamara
, who used the concept while he was president of Ford Motor Company to force the various divisions of the automaker to streamline corporate workings. Shapley
says that McNamara
later used the same phrase to describe his strategy of playing off the armed services against each other. Enthoven
, however, dismisses this etymology as "fanciful" and "preposterous," and maintains that he came up with the term for his health-care system himself, in 1986."
- Rand Corporation Theoretical Models
guided the effort (after 1955 - as it became governmentally declassified)
- Hired PhD's from Academia and ROTC Lieutenants in areas judged worthy disciplines
- Looked at the "Larger Picture" at the expense of the local details (?"Academic Strategy")
- Henry Linn, Albert Woftedder , Harry Rowan, Fred Hoffman, Les Aspen PhD (Oxford, MIT )
- Robert McNamara (Manage from the Grand Totals Down, not Details Up).
- This approach creates a view that is invisible to those not in the top echelon, and ignores their inputs ("Ruling Elite").
- Pentagon Defense
utilization program sources
- Grouped Weapons systems by their Budgets and tied those Budgets to Goals
- Academic Strategy and Prediction approach - Tactics replaces Strategy
- Charlie Hitch (1959 Nuclear strategy, weapons systems analysis team concept)
- Joe Peck, David Steager
, Vick
Heyman
- Alain Enthoven
is an important figure in theoretical models for centralized control systems. His hour long interview from 2010 provides a framework for understanding how we got here and what is fueling it. "Conversations of History" (136-01)
- Understanding driving forces behind this scheme and how it has left Medicine in rubble;
- Managed Competition Principles
- Fundamentally
Managed Competition
is based on Academic Theory
- It relies on Theory and Computer Modeling - but seldom is testable
- Augments Credibility by providing Theoretical Gravitas
, giving power to dominate decision making with little ability to challenge (Academic Degrees)
- May encourage
decisions that are rationalized or made by "Wishful Thinking."
It requires a constructed ignorance of the local conditions.
- Managed Competition in Health Care - Use of Non-Physicians
( 22-01 ) 22-01a putting non-physicians in charge. pdf <<< EXPAND
- Fundamentally
Managed Competition
is based on Academic Theory
- Health Care Highlights to Note
- Changes in the U.S. Health Care have
required enormous increases in Administrative Overhead Costs
.
- "Reluctance to consider other options seriously over time may stem partly from the support that the Clinton campaign received from the managed care sector of the private insurance industry, as well as from a
perception that simpler and more popular options, including a single-payer approach, are unlikely to pass in the U.S. Congress
."
- "The only
countries that have successfully contained costs are those using single-payer financing
.
"
- "Rats and roaches live by competition under the law of supply and demand; it is the privilege of human beings to live under the laws of justice and mercy. It is impossible not to notice how little the proponents of the ideal of competition have to say about honesty, which is the fundamental economic virtue, and how very little they have to say about community, compassion, and mutual help
."
- CBS 60 Minutes has recently reported on [drug and equipment supplier] McKesson's complicity in the Opioid
Crisis
. Enthoven
spent four years as a director and stockholder of PCS, Inc., a "pharmaceutical managed care" company that was taken over by the drug distribution giant McKesson Corporation in 1989. "In its 1993 annual report, McKesson noted, 'With PCS, [we are] in a prime position to benefit from the rapid growth of managed-care health plans.'
( 23-01 ) 23-01 1MotherJones MJ93/ The godfather of managed competition | Mother Jones.pdf
- Changes in the U.S. Health Care have
required enormous increases in Administrative Overhead Costs
.
- Origins of Managed Competition
-
Alain Enthoven
, protege of Robert McNamara
(Ford Motor Company)
********* \/ If you read anything, READ THIS***************** !!!!!
23-01 EnthovenSumm1HL.pdf <<<OPEN (Review Article - 29 pages)
References for Article:- "
Is Managed Competition the Answer
" - Mother Jones - 1993
https://www.motherjones.com/politics/1993/05/motherjones-mj93-godfather-managed-competition/ - "
Computers, Electronic Data and the Vietnam War
" - Donald Fisher Harrison
- 1994
https://archivaria.ca/ index.php / archivaria /article/view/11490/12434 - "
Alain Enthoven
: An Outspoken Champion for the Prepaid Group Practice
" - 2004
https://www.ncbi.nlm.nih.gov/ pmc /articles/PMC4690696/ - "
The Strange Career of Managed Competition: From Military Failure to Medical Success?"
- 1994
http://connection.ebscohost.com/c/articles/9406150705/ strange-career-managed-competition-from-military-failure-medical-success - "
Alain Enthoven
states that single payer may be inevitiable
" - 2003
http://www.pnhp.org/news/2003/ september / alain-enthoven-states-that-single-payer-may-be-inevitiable
- "
Is Managed Competition the Answer
" - Mother Jones - 1993
- Bill Clinton Task Force 1993
/"Hillary Care"
- The Forward to the Clinton Presidential Task Force Report is telling regarding a Single Payer Plan.
1993 Presidential Task Force Foreword (download pdf): 1993 Health Care Reform.pdf <<< OPEN
- "a single-payer system might achieve the goals of health care reform as well as - or better than - the form of managed competition with a budget that has emerged from the Presidential Task Force. However, a single-payer system imposed by the federal government may not be politically feasible... In fact, it may never have been feasible given the deeply entrenched American patterns that tie health care to employment and the insurance industry
."
- "a single-payer system might achieve the goals of health care reform as well as - or better than - the form of managed competition with a budget that has emerged from the Presidential Task Force. However, a single-payer system imposed by the federal government may not be politically feasible... In fact, it may never have been feasible given the deeply entrenched American patterns that tie health care to employment and the insurance industry
."
- Bill Clinton empaneled a Task Force to craft Health Reform. Contrary to common belief, "by the time Hillary [Clinton] became involved in health-care reform in late January 1993, Bill Clinton's thinking about the problem was already well advanced. He had settled on the basic model for reform -- "a plan for universal coverage based on consumer choice among competing private health plans, operating under a cap on total spending", an approach known as "managed competition within a budget".
- The decision meetings about the plan took place outside the formal structure of the task force, usually in the Roosevelt Room of the White House, and the president ran the meetings himself.
- The President's Task Force -- consisting of members of the cabinet and several other senior officials -- proved to be useless for reaching decisions and drafting the plan. It immediately became the subject of litigation and dissolved at the end of May without making any recommendations.
- Ira Magaziner
is best known for leading, along with Hillary Clinton, the failed Task Force to Reform Health Care in the early Clinton administration. Brad DeLong
, Deputy Treasury Secretary for the Clinton administration at the time, argues that Magaziner's
failures stemmed from having a background in management consulting instead of policy." Magaziner
was court ordered to pay $285,864 to the Association of American Physicians and Surgeons, in 1997 by a federal judge for lying about whether the Task Force to Reform Health Care hired non-governmental employees and therefore had to release documents from their strategic deliberations upon public request. The fine was later overturned on appeal on August 25, 1999.
- The concept of 'health decided by wealth' - can not work when the government bears responsibility for the costs, because of an inherent inability to predict who requires more resources before-hand. Tying care to employment and to insurance is a death blow.
- Paul Starr
has written extensively and an often sited resource on Health Care Reform. Here is an article written on his perspective of the Health Reforem
in the Bill Clinton Administration:s
( 146-01 ) The Hillarycare Mythology HL.pdf <<<OPEN
- The Forward to the Clinton Presidential Task Force Report is telling regarding a Single Payer Plan.
- There is a need additionally to Examine the Concept of The "Free" Market and its Corporate Interpretations
- Milton Freedman
championed flawed economic theory (Neo-Liberalism, the Free Market would rule all).
- Business is more efficient than Government in running services for the people
- Centralized Governmental Limitations on Individuals
- Collapse of Brazil, Venezuelan Economies under Gross Free Market Policy
- Allows lawless Corporate dominance (used to be termed Laissez-Faire)
- Milton Freedman
championed flawed economic theory (Neo-Liberalism, the Free Market would rule all).
back
back
-
Taxes paid by Industry Sector
Ranking America’s industries by profitability and tax rate
( 140-40 ) 140-40 Ranking America’s industries by profitability and tax rate _ FT Alphaville.pdf
"Across the American private sector, companies pay about 15.5 per cent of these earnings in net tax ."
- Taxes paid Rankings by edidta
margins by industry
140-40b ebidta margins by industry.pdf
-
Taxes paid Rankings by Gross Output by Industry
140-40a taxes by gross graphic.pdf -
- Taxes paid Rankings by edidta
margins by industry
-
Forms of Taxation to Consider
-
GROSS RECEIPTS TAX
( 117-02 ) 117-02 tax pyramiding sr147. pdf <<<OPEN
-
As the name suggests, a gross receipts tax is a
tax imposed on all business sales
. In the United States, gross receipts taxes were first introduced at the state level in the early 1920s. According to 2015 report by the tax consulting firm CBIZ
, gross receipts taxes were in operation as of 2015 in Texas, Ohio, Washington, Delaware, and Washington.
-
Gross Receipts Tax is a
stable source of revenue with a broad base, low rate, and low administrative cost.
- It is a Tax on the Seller
, proportionally adds to any sales tax.
- Their simple structure makes them easy for states to administer and for companies to comply with
, in contrast to notoriously complex state corporate income taxes (decreased overhead costs).
- As an expansive broad base of all transactions in the economy, they are able to raise a given amount of revenue at lower rates than any other tax
, making them politically attractive to lawmakers.
-
"A gross receipts tax has the highly favorable feature that it
creates no disproportionate burdens on businesses whose operations rely more on employing workers as opposed to relying more on utilizing expensive machinery and buildings
(i.e. “capital plant and equipment”) to produce goods and services. That is, a gross receipts tax does not discriminate in its impact between more “labor-intensive” firms as opposed to more “capital-intensive” firms."
( 15-0 ) 15-0 Pollin-Economic-Analysis-SB -562 HLa.pdf
- "This is in contrast with a payroll tax, in which the tax base is established according to the total amount of wages a business is paying to its workers. A payroll tax therefore favors firms that heavily utilize machinery as an alternative to hiring people to conduct its operations ."
- A Gross Business Tax would not include Securities transactions, which are a separate
source of income for some Californians.
-
Gross Receipts Tax
- Issues of Tax Pyramiding
-
There are issues with a Gross Receipts (Business, Excise, Productivity) Tax, leading to frequent voiced objections.
(117-02) 117-02 tax pyramiding sr147. pdf <<<OPEN
- Tax pyramiding occurs when taxes are imposed at each stage of production, creating an extra layer of taxation
at each stage of production. This results in multiple layers of taxation on the same goods
. Costs earlier in the production trail are taxed at a higher rate
than at the end of production at sale.
(117-02)
117-02 tax pyramiding sr147.
pdf
<<<OPEN
- If your company is operating at a net loss, but you have revenue from sales, you may have to pay the gross receipts tax based on the amount that you collect from customers. However, sales of food and exempt consumables are exempted in varying easy in other single payer program and have been included in the CNA
supported SB-562/2.3 plan.
( 122-03 ) 122-03 Difference Between Sales Tax & Gross Receipts Tax _ Chron.pdf
-
There are issues with a Gross Receipts (Business, Excise, Productivity) Tax, leading to frequent voiced objections.
-
Lawmakers turned to sales and gross receipts taxes as emergency revenue sources at the onset of the Great Depression in 1929.
-
As the name suggests, a gross receipts tax is a
tax imposed on all business sales
. In the United States, gross receipts taxes were first introduced at the state level in the early 1920s. According to 2015 report by the tax consulting firm CBIZ
, gross receipts taxes were in operation as of 2015 in Texas, Ohio, Washington, Delaware, and Washington.
-
SALES TAX (buyer tax)
-
Sales tax is collected by the retailer when the final sale in the supply chain is reached via a sale to the end consumer. End consumers pay the sales tax on their purchases. Businesses issue resale certificates to their sellers when buying business supplies/inputs that will be resold since sales tax is not due. Tax jurisdictions do not receive the tax revenue until the sale is made to the final consumer. (128-01)
-
Sales tax is collected by the retailer when the final sale in the supply chain is reached via a sale to the end consumer. End consumers pay the sales tax on their purchases. Businesses issue resale certificates to their sellers when buying business supplies/inputs that will be resold since sales tax is not due. Tax jurisdictions do not receive the tax revenue until the sale is made to the final consumer. (128-01)
-
INCOME TAX (corporate, buyer taxes)
-
Many complain that Corporate tax rated are too high. Data from the Tax Foundation itself indicates that actually all the big economies have tax rates above 30%. The United States is a corporate tax haven (2017)
, with the lowest effective corporate tax
rates of almost all the countries that participate in the Organisation
for Economic Co-operation and Development (
OECD
). Data from the
OECD
show that in the average member country corporate taxes are equal to about 3.5 percent of GDP. In the United States, corporate taxes have generally been between and 1.5 percent and 2.5 percent of GDP over the last two decades, according to the
Congressional Budget Office.
-
Over the last 60 years, the U.S. tax code has dramatically shifted away from corporate taxes and toward taxes on individuals, especially through the payroll tax, the financing backbone of Social Security and Medicare. In the 1950s, the corporate income tax brought in, on average, one of every four dollars in federal tax revenues. By the 2000s, however, it raised just one of every 10 tax dollars.
- The shrinking share of corporate taxes was made up by an increase in payroll taxes which funded social insurance and retirement programs. Excise and other taxes—such as fuel taxes, phone taxes, etc.—shrank as well over the last 60 years, while the individual federal income tax rose slightly, from an average of 43% of total federal revenue in the 1950s to 46% in the 2000s. Only the "less favored" pay taxes. Over the period in which the progressivity
of the tax system declined, pre-tax income inequality grew significantly. Employers paid less for their workers.
-
Increases in corporate tax rates lead to lower future growth rates within countries. The coefficient estimates suggest that a cut in the corporate tax rate by ten percentage points will raise the annual growth rate by one to two percentage points.” It is a fools bargain.
-
It is very likely that a lot of the effects of income tax cuts is from non-wage income. That is, tax-cuts (or increases) stimulate economic growth (or decline) on lower wage earners and so are paid for. Hi-income (investor) tax cuts have little stimulatory effect. In Hungry for example, a tax cut at high incomes did
not
boost taxable income dramatically.
- Lower overall
rates, with fewer loopholes by which to not pay them could be beneficial:
- more government revenue
- a fairer playing field for businesses
-
a more predictable and less corrupt business environment, in which both investors and consumers could plan for the future with more confidence. Investors may make more profit in times of large asset fluctuations, whereas workers make more profit in times of stability.
-
SB-562 may be similar to a sales tax on entire economic activity, and comparisons to Gross Business Tax attempts in other States or settings can be instructive. But there is a significant difference from other excise taxes on individual industries.
( 119-04 )
- First, health care would be delivered to every resident of the State. The benefit flows back to every Resident from a tax on all Residents, based on consumption. It is a tax on everybody flowing back to everybody.
- A Tax abatement for an individual company such as Motorola in Pheonix moving to town inverts this. It extracts tax revenues from the entire population and sends the benefit to a smaller group - those who buy Motorola products or the company that produces it. This also nets amplified Pyramided cost savings; cash savings allows immense borrowing on margin to crush competition.
-
This transfer of public wealth in a region of decreased environmental restrictions also lowers corporate costs at the expense of the environment.
-
Many complain that Corporate tax rated are too high. Data from the Tax Foundation itself indicates that actually all the big economies have tax rates above 30%. The United States is a corporate tax haven (2017)
, with the lowest effective corporate tax
rates of almost all the countries that participate in the Organisation
for Economic Co-operation and Development (
OECD
). Data from the
OECD
show that in the average member country corporate taxes are equal to about 3.5 percent of GDP. In the United States, corporate taxes have generally been between and 1.5 percent and 2.5 percent of GDP over the last two decades, according to the
Congressional Budget Office.
-
VALUE ADDED TAX - VAT
(
buyer tax
)
- This is a type of Gross Transaction Tax but with refunding. A VAT tax is a tax imposed on all the steps in the process of making, distributing and selling a product. The VAT (Value-Added Tax) is collected by all sellers in each stage of the supply chain. Suppliers, manufacturers, distributors and retailers all collect the value added tax on taxable sales. Suppliers, manufacturers, distributors, retailers and end consumers all pay the VAT on their purchases. Businesses must track and document the VAT they pay on purchases that will be resold and receive a credit for the VAT paid on their tax return, so that the consumer ultimately pays the tax. s. Tax jurisdictions receive the tax revenue throughout each step of the supply chain as opposed to only at the sale to the final consumer chain, but it generates the same amount since the extra payments are ultimately refinded
. (128-01, 129-02)
- This is a type of Gross Transaction Tax but with refunding. A VAT tax is a tax imposed on all the steps in the process of making, distributing and selling a product. The VAT (Value-Added Tax) is collected by all sellers in each stage of the supply chain. Suppliers, manufacturers, distributors and retailers all collect the value added tax on taxable sales. Suppliers, manufacturers, distributors, retailers and end consumers all pay the VAT on their purchases. Businesses must track and document the VAT they pay on purchases that will be resold and receive a credit for the VAT paid on their tax return, so that the consumer ultimately pays the tax. s. Tax jurisdictions receive the tax revenue throughout each step of the supply chain as opposed to only at the sale to the final consumer chain, but it generates the same amount since the extra payments are ultimately refinded
. (128-01, 129-02)
-
TAX CREDIT / TAX DEDUCTION
(entity tax)
- Many of the fundamental economic connections that affect individuals are not transparent. An example is the distinction between a credit and a deduction. Health Care needs to be a credit - an asset available based on the need, not a deduction, an asset which is some percentage of "taxable earnings". Many complain about the pyramiding of taxation
. Yet at the same time they promote the pyramiding of profit
. Stock options complicate financial discussions because the ratios of benefit and liability to employer/employee/taxpayer are variable and pushed off into the future.
- Many of the fundamental economic connections that affect individuals are not transparent. An example is the distinction between a credit and a deduction. Health Care needs to be a credit - an asset available based on the need, not a deduction, an asset which is some percentage of "taxable earnings". Many complain about the pyramiding of taxation
. Yet at the same time they promote the pyramiding of profit
. Stock options complicate financial discussions because the ratios of benefit and liability to employer/employee/taxpayer are variable and pushed off into the future.
- It is true that taxes are written into corporate ledgers as a "cost of production" and are added to the cost of the final product. The consumer pays anyway in the end. However, what is not clear is that each step of production which is not
taxed is in effect a taxpayer subsidy. Each activity gets a tax-free discount. In that way, employers are less affected by the societal costs of each transaction. Taxing each step of production a little ties the revenues to actual production costs and benefits, rather than hidden asset, finance and tax manipulations that become divorced from actual production. In addition, services such as by a plumber, would be taxed once. The physical pipes used would be taxed at each production activity. Each step of production pays a little (smaller) load of the total tax. A zero corporate tax gives governmental leverage to corporations. The larger the corporation, the greater the leverage relative to individuals.
-
GROSS RECEIPTS TAX
back
back
-
General Comparisons of Quality
(Commonwealth Fund 2014)
-
The
United States ranks last overall
among 11 industrialized countries in 2014, dragged down substantially by deficiencies in access to primary care and inequities and inefficiencies in our health care system
. The US was also last in 2004, 2006, 2007, and 2010 rankings. The U.K
. and Switzerand
rank the best, but at half the cost.
( 137-01 ) 137-01 US Health System Ranks Last Among Eleven Countries on Measures of Access, Equity, Quality, Efficiency, and Healthy Lives - The Commonwealth Fund.pdf
-
US Healthcare Rankings 2014 (Australia, Canada, France, Germany, the Netherlands, New Zealand Norway, Sweden Switzerland, United Kingdom, United States)
- 3rd - Effective Care
- 4th - Patient-Centered Care
- 5th - Quality Care, Timeliness of Care
- 6th - Coordinated Care
- 7th - Safe Care
-
11th - Overall, Cost Problems, Efficiency, Equity, Healthy Lives,
-
People in the U.S. have the hardest time affording the health care they need. It has the most expensive health care system (twice per capita other countries).
-
The U.S. ranks last on infant mortality, and on deaths that were potentially preventable with timely access to effective health care. It ranked second-to-last on healthy life expectancy.
- The U.S
ranks last in efficiency, due to low marks on the time and dollars spent dealing with insurance administration; lack of communication among health care providers; and duplicative medical testing.
- Forty percent of U.S. adults who had visited an emergency room reported they could have been treated by a regular doctor, had one been available. This is more than double the rate of patients in the U.K
.
- People in the U.S. have the hardest time affording the health care they need. It has the most expensive health care system (twice per capita other countries). The U.S. ranks last on every measure of cost-related access. More than one-third (37%) of U.S.adults
reported forgoing a recommended test, treatment, or follow-up care because of cost.
- The U.K
. with a completely socialized system, provides a ranked #1
overall.
-
Canada
ranks next to last overall, but is
better than the the United States which is last
.
- These rankings indicate
a need to do something. A universal health system has definite cost advantages; an argument can be made to employ Physicians for Primary care (everybody needs and give stability), with fee-for-service for Specialty care. However, Primary Care compensation must be robust, and without fee-for-service for all providers, care migrates into Specialty Care. Managed Care does not save money because it increases the Administrative Cost for All Care, regardlesss
of the Cost for Primary Care, and limits access to Specialty Care.
-
Findings of studies at Dartmouth highlights that more medical care is not necessarily better for chronic care:
-
There was little difference in the risk of death among newborns in regions with the lowest and highest levels of neonatal intensive care unit (
NICU
) beds. The risk was somewhat greater in regions with the lowest numbers of Neonatologists
compared with regions with somewhat higher numbers of neonatologists
. However, little additional benefit in survival was seen with further increases in the supply of Neonatologists
. Increased Medicare spending (60% in the higher hospitals) is not associated with improved survival, ability to engage in daily activities, quality of care, or satisfaction with care.
-
Medicare pays some California hospitals
four times more
than others to care for patients with similar chronic illnesses, with no gain in quality or patient satisfaction, according to a study. The additional care provided in some regions and hospitals did not improve medical outcomes or patient satisfaction? in fact, as the volume of care increased, the quality of care and patient satisfaction declined.
- "The higher use found in California, as elsewhere, reflects a delivery system in which services are driven not by patient need, but by the relative availability of resources
. In regions that have more hospitals, more ICU beds, more physicians and more specialists, patients receive significantly more services at greater cost, but with no improvement in outcomes."
- "Medicare faces a serious 'overuse' problem, which is significant given its fiscal problems," says John E. Wennberg , M.D., M.P.H ., the study's principal investigator and director of the Center for the Evaluative Clinical Sciences at Dartmouth Medical School in Hanover, NH.
-
There was little difference in the risk of death among newborns in regions with the lowest and highest levels of neonatal intensive care unit (
NICU
) beds. The risk was somewhat greater in regions with the lowest numbers of Neonatologists
compared with regions with somewhat higher numbers of neonatologists
. However, little additional benefit in survival was seen with further increases in the supply of Neonatologists
. Increased Medicare spending (60% in the higher hospitals) is not associated with improved survival, ability to engage in daily activities, quality of care, or satisfaction with care.
-
The
United States ranks last overall
among 11 industrialized countries in 2014, dragged down substantially by deficiencies in access to primary care and inequities and inefficiencies in our health care system
. The US was also last in 2004, 2006, 2007, and 2010 rankings. The U.K
. and Switzerand
rank the best, but at half the cost.
-
Canada - Worth A Look?
-
"Canada’s health-care system is third-last in new ranking of developed countries." (with concerns also in other rankings). However:
( 150-01 ) 150-01 Canada’s Single-Payer Health Care System_ A Cautionary Tale _ National Review.pdf> <<<OPEN
- One recent article in National Review descibes terrible Health Care in Canada. The article, in a magazine which has a long history of antagonizm to publically funded Health Systems, is laced with loaded, negative exclamations but short on facts. It criticises the Canadian System in a way that is representative of such criticisms.
- Well, maybe so. The Canadian Health System does have have some problems - until you realize it is consistently ranked higher than the United States .
- "The Canadian system is Universal and Affordable ."
- "in Canada health care is technically delivered privately, although given the Kafkaesque regulations and restrictions that govern it, the system is by no means market-based."
- "While medical providers are independent from the federal government, they are compelled to accept CHA insurance —and nothing else — by a prohibition on accepting payments outside the national-insurance scheme so long as they wish to continue accepting federal health-transfer funds ."
- "In Canada, the government determines what procedures are medically necessary". CA SB-562 empowers a Board, not the Government with this task, and will be the subject to judicial challenge, unlike in Canada.
- The costing citied
in the article does not appear to agree with other sources of data.
-
"Canadian doctor to U.S.: Try single-payer health care instead of trashing it"
( 150-02 ) 150-02 -Canadian doctor to U.S.pdf <<<OPEN
- "In Canada, the notion that access to health care should be based on need , not ability to pay, is a deeply ingrained value."
- "The single-payer, publicly funded health care systems in Canada cover virtually every resident of our country, at a much lower cost than the U.S. "
- " Canadians live longer than Americans , and according to a recent study published in The Lancet , the Canadian system outperforms the U.S. on quality and access to care overall ."
- "It’s true that sometimes Canadians wait too long for nonurgent or elective investigations or procedures.... Most importantly, Canadians don’t wait for urgently-needed care. When Canadians get sick they get the care they need, and the care they get is good."
-
"Single-payer health care is also much less administratively onerous and expensive. The billing office in the clinic where I work serves more than 40 primary care doctors, and employs only two billing clerks — because billing is so simple. Every month my practice sends one bill to the public insurance plan, and every month we get paid on time."
-
"Canada's Single Payer Health Care System - It's Worth a Look"
( 150-03 ) 150-03 -Single Payer Health Care System.pdf
- The Canadian system is a publicly funded insurance program where costs are controlled and both hospitals and doctors are private .
- "the single payer system that Canada has used for the last 25 years has drastically simplified their administration costs . For instance, it takes more people to administer Blue Cross Blue Shield of Massachusetts that it does to administer the entire health care system of Canada. Before Canada implemented their national health program, their health costs were the same portion of their economy as in the U.S. After they implemented their program, their costs stabilized at 9% while U.S. costs have increased to 14%. They spend one tenth of what U.S. health care providers spend on overhead."
- "Since the wealthy as well as the middle income people have no alternative, they make sure it is funded adequately. This together with cost controls insures that everyone including the poor, who use the same system, receives the same high quality care."
-
Canada does appear to not adequately tax young boomers
for their anticipated care needs - something similar to plans by the current U.S. Congress to tax older americans
at 5 times the rate of younger. That is, our system borrows heavily to provide, with the actual costs mounting under the radar. Much as in the U.S., however, care is being privatized for profit, with the added overhead fees charged to patients going to the private companies.
- The Impact of Single-Payer Health Care on Physician Income in Canada, 1850–2005 (2011)
( 149-15 ) 149-15 AJPH2010350_ Duffin.indd - 1198. pdf
"The universal, single-payer system has been good not only for Canadians but also for their doctors. At least, it has done no harm."
-
Recently, forces in Candada
are pushing to privatize the Insurance components of Canadian Health Care
. It appears to be an attempt to monetize their lower costs, skimming off the resultant increased out-of-pocket cash into private profit. Essentially, they are moving to the more costly American System of excess Cost.
-
"Canada’s health-care system is third-last in new ranking of developed countries." (with concerns also in other rankings). However:
-
How does the U.S. Healthcare Compare to the World?
- The 10th annual global Prosperity Index was issued by the The Legatum
Institute, a London-based research institute, a huge survey that ranks the most prosperous countries in the world. One of the big components of the ranking is how healthy a country's people are.
( 151-15 ) 151-15 The 16 countries with the world's best healthcare systems - Business Insider Nordic.pdf << OPEN
( 151-15a ) 151-15a prosperity report.pdf << OPEN
- Perhaps unsurprisingly, the countries that have the best scores in the Prosperity Index, and therefore rank as the world's healthiest, are generally big, developed economies with large amounts of resources.
- Britain — whose NHS pioneered free at the point of use healthcare globally — finishes 20th in the Legatum
Institute's health sub-index. The U.S. ranks further down.
-
World Health Organization Rankings (WHO 2017)
-
Highest Ranked Countries
-
U.S. and Canada Ranking (2017)
-
Highest Ranked Countries
-
The United States has
fewer Physicians per Capita
compared to many Countries (AAMC
).
177-07 Feb13_ Michener.pdf <<< OPEN SOURCE
177-07 per capita lower.pdf <<< EXPAND
- Number of doctor visits per capita
in selected countries as of 2015
( 178-01 ) 178-01 MDpercapitaGraphic.pdf
- The Supply of Physician Services in OECD
Countries - Supply of General Practitioners.
( 177-01 ) 177-01 35987490. pdf <<< OPEN SOURCE
-
The higher the number of General Practitioner Physicians Per Capita, the fewer the Number of Visits per General Practitioner.
177-02 gp visits per gp.pdf <<< EXPAND
- Although each General Practitioner Physicians may see fewer patients, patients have more visits to General Practitioner Physicians when there are more General Practitioners Per Capita
.
177-05 number gp visits per gp.pdf <<<EXPAND
-
"The role of Specialists versus Primary Physicians is still unclear."
177-04 md specialization trendsa.pdf
-
The higher the number of General Practitioner Physicians Per Capita, the fewer the Number of Visits per General Practitioner.
-
Conflicts in planning for the Health Care Workforce - hard to do.
177-06 limitations of workforce planning.pdf
- The 10th annual global Prosperity Index was issued by the The Legatum
Institute, a London-based research institute, a huge survey that ranks the most prosperous countries in the world. One of the big components of the ranking is how healthy a country's people are.
-
More Doctors Better Care?
- The scatter plot in Figure 1 below illustrates that there is no association between avoidable mortality and overall physician supply (relative to Canada)
. Similar plots illustrate that there is also no relationship between avoidable mortality (a) general practitioners and family physicians per capita, (b) specialists per capita, (c) nurses per capita, (d) doctors and nurses per capita or (d) health expenditures per capita, though the ordering of countries changes depending on which indicator is used (graphics available at
www.chspr.ubc.ca
).
( 179-01 ) 179-01 policy-05-026. pdf
Of note, no countries with lower rates of physicians-per-capita than the U.S. had better mortality rates.
179-01a md supply mortality graphic.pdf
- This indicates that other other factors may be involved in overall mortality differences. One thing to consider is the ability to diagnose what is an avoidable death. And comparing Maternal Mortality Rates, many of the same countries that have the greater number of physicians per capita show up with extremely low mortality rates. The US ranks worse in Maternal Mortality than some 50 other countries, with 3-7 times the maternal mortality rates
: (
181-01
)
- 181-01a Maternal Mortality Lowest.pdf
- 181-01b Maternal Mortality USA.pdf
-
(
182-05
) 182-05a Maternal Mortality Rising Graphic.pdf
-
Additional conversations:
182-03
,
182-06
,
182-07
182-08
,
182-09
,
182-10
- 181-01a Maternal Mortality Lowest.pdf
-
Perhaps trying out a Single Payer Universal Health Care System in California, such as the SB-562 proposal, could be of benefit, making us less than a third world country in results.
- Now that the Corporate/Academic changes to Healthcare have once again proven to increase costs, the Hospital Systems are moving to hide the fact by Mergers and re-organization under
"ACO
-2".
- "In the US, we haven’t bothered to create national health policies around maternity care that are focused on improving outcomes for mothers, such as a federal maternity leave policy or universal health care
.
"Maternal health is also becoming more complicated. The clinical complications CMQCC has focused on so far — hemorrhage, preeclampsia — are being outpaced by lifestyle-related health issues , like cardiovascular disease and opioid addiction . There are also astounding racial disparities in maternal health: Black mothers are three times more likely to die in childbirth than white women. It’ll require more than well-meaning doctors and nurses to fix these problems." This may belweather the need for more trained Physicians, not fewer. ( 182-02 )
-
"the vast majority of undocumented residents in California are adults, and expansions of affordable insurance coverage for this group still face major hurdles. Despite the likelihood of continued legislative efforts next year, the costs of covering adults and the uncertainty of federal actions make it difficult to predict success. In the absence of these major federal and state reforms, undocumented adults without health insurance will continue to rely on safety net providers and county indigent care programs for needed health services.
"Several counties do not cover the undocumented under their indigent care programs. Our estimates suggest nearly 900,000 undocumented residents in California live in counties where they are not eligible for county indigent care programs . These exclusions place additional strains and financial responsibility on local health care systems—including hospital emergency departments and community clinics— in these regions. Moving forward, it will be important for the state to support local safety net providers and consider providing incentives or direction to counties to include the undocumented under their indigent care programs. Even so, the limited programs and safety net resources currently available to uninsured undocumented immigrants still do not equate to comprehensive health insurance coverage." ( 182-01 )
- Now that the Corporate/Academic changes to Healthcare have once again proven to increase costs, the Hospital Systems are moving to hide the fact by Mergers and re-organization under
"ACO
-2".
- The scatter plot in Figure 1 below illustrates that there is no association between avoidable mortality and overall physician supply (relative to Canada)
. Similar plots illustrate that there is also no relationship between avoidable mortality (a) general practitioners and family physicians per capita, (b) specialists per capita, (c) nurses per capita, (d) doctors and nurses per capita or (d) health expenditures per capita, though the ordering of countries changes depending on which indicator is used (graphics available at
www.chspr.ubc.ca
).
back
back
- Annual Health Spendings
in the U.S. / California
- Annual Spending comparison.
- The Annual U.S. GDP is about $76 Trillion dollars. (2017)
- The Annual California GDP is about $11 Trillion dollars . (2017)
- The Annual California Health Care spending is about $370 Billion dollars. (2017)
- The Annual California State Budget spending total
is about $270 Billion
dollars
.
(2017)
- California Annual Health spending
totaled
$292 billion in 2014
— 12.6
%
of the state's economy
(
$370 billion in 2017
)
.
- "Health spending per capita in California ($7,549 ) was lower than the US average ($8,045 ), and ranked 15th among all states in 2014 (the state with rank of 1 is least expensive).
- Health spending growth averaged 4.9% per year in total and 4.0% per capita from 2009 to 2014. This was faster than average US spending growth (3.9% total health spending, 3.1% per capita). Growth is even higher since 2014.
- California Health Spending increase
exceeded California's average annual five-year growth in GDP (4.2%) in 2014
; CPI (1.9%
) and median wage (1.0%
) increases were seen.
- Health Spending by Funding Source in California (2014)
- Annual Spending comparison.
- A small number of patients use half
of the US Healthcare dollars spent
http://www.oracle.com/us/industries/018896 . pdf ( 140-14 ) <<OPEN
http://www.healthcarefinancenews.com/news/cost-sharing-may-not-cut-health-costs ( 140-09a 5% cost 50% , 140-09b employee cost ) <<OPEN
- 5% of the population accounts for almost half of every healthcare dollar spent annually
.
Two-thirds of these expenditures are by those over 50 years old.
80% of health care costs are driven by just 19%
of the population. This encourages healthy people to avoid health care insurance purchase.
- Hyper-managing younger patients thus cannot improve costs.
Excluding a buy-in for younger patients will only worsen Health finances when they become older or sicker. Increasing cost sharing for these sick individuals forces them into less-comprehensive or more expensive insurance. "
It is critical to focus instead on these very sick and chronically ill patients
," perhaps by using better trained and paid providers?
- Also increasing Electonic
Data Access to the other 95% can only predictably increase cost thru increased overhead because there are no costs to save!
Perhaps we should use a more selective electronic system
to share the high risk information, not universal gigantic programs?
- Two cost-sharing policies: the Affordable Care Act's excise tax on high-priced employer-sponsored health insurance
, and the proposal to restructure Medicare into a voucher program have been attempted. For those who need extensive medical care, both of these policies may result in financial distress or sacrificing medical treatment
. Ultimately, any cost containment achieved by making healthcare more expensive to consumers is driven by reduced medical care, not reduced prices
. “They may even cut back on medical spending that is cost effective in the long run.”
- “These policies may ease the federal budget, but research shows that they will do little to contain overall health spending
,
” the report said. “Furthermore, they put all the burden of cost containment on consumers without giving them the tools to make more fully informed medical decisions.”
- 5% of the population accounts for almost half of every healthcare dollar spent annually
.
Two-thirds of these expenditures are by those over 50 years old.
80% of health care costs are driven by just 19%
of the population. This encourages healthy people to avoid health care insurance purchase.
- Rising Health Costs
- HRI
(
Pwc
Health Research Institute - Accounting Services
) projects 2018’s medical cost trend increase at +6.5%
—the first uptick
in growth in three years.
( 140-03 ) 140-03 hri-behind-the-numbers -2018. pdf
( 140-03a ) 140-03a 2017 Health and Well-being Touchstone Survey results_ PwC.pdf
( 140-03b ) 140-03b Behind the numbers 2018_ PwC.pdf
- Now that the fiscal irresponsibility
of American Hospital Administration and its self-aggrandizing policies that pretend to control costs is becoming more visible (
Hospitalists
add $200,000 a year each, Nurse Practictioners
cost just as much and more that Primary Care Physicians), the consequences of Vulture Capitalism must kick in. As well, salary inflation of artificially suppressed providers also kicks in.
he Medical Corporations are scrambling to hide the Fiscal Irresponsibility by new Mergers, consoliations and Re-Organization (was termed " Re-Engineering " in the 1990's).
- Part B Medicare Supplemental Premiums are expected to rise in 2018. ("
MediGap
).
- 70% of beneficiaries
who enrolled in Medicare before 2017 are protected by a hold harmless rule, and will pay premiums ranging from about $110 to $126 per month
. This is 25% of the cost share
shouldered by those paying the standard Medicare premiums. Social Security recipients covered by the hold harmless rule will see a monthly benefit increase of $25, but that will not cover the increase in Medicare Part B premium
.
( 109-01 ) 109-01 2016 tax returns determine 2018 Medicare premiums.pdf
( 109-02 ) 109-02 Medicare premiums may devour increased 2018 Social Security benefit.pdf
- For Beneficiaries with incomes around $150,000
,
premiums are expected to rise from $238 per month to $310 per month in 2018
, which raises Medicare premiums to cover 65 percent of program costs (up from 50 percent) for beneficiaries in this income bracket.
- For Beneficiaries with incomes around $190,000, monthly Part B premiums are expected to rise from $310 to $381 in 2018, covering 80 percent of program costs
(up from 65 percent).
- High-income individual surcharge for Medicare Part B range from $187.50 to $428.60 per month. Individuals whose income topped $214,000 per individual in 2015 will pay more than $5,000 each for Medicare Part B premiums alone in 2017. That represents 80% of the per capita cost of the Medicare Parts B and D programs
.
- (
109-03
) Kaiser Family Foundation analysis 109-03 Medicare’s Income-Related Premiums Will Rise for Some Higher-Income Beneficiaries Beginning in 2018 _ The Henry J.pdf
- 70% of beneficiaries
who enrolled in Medicare before 2017 are protected by a hold harmless rule, and will pay premiums ranging from about $110 to $126 per month
. This is 25% of the cost share
shouldered by those paying the standard Medicare premiums. Social Security recipients covered by the hold harmless rule will see a monthly benefit increase of $25, but that will not cover the increase in Medicare Part B premium
.
- To slow healthcare spending growth moving forward, employers
will consider supplyside
management strategies -such as narrower provider networks and value-based purchasing—that focus on bringing price, rather than utilization, down.
- There will be more individual cost-sharing. Participants are using Preferred Provider Organizations (
PPOs
) less, and High Deductible Health Plans
(
HDHPs
) more.
- High Deductible plans
- We will not cover a great deal about high deductible plans, except to say that when combined with an HSA Health Savings Account , 100% of the savings is from the Tax savings on the HSA contributions. HMO's have savings from low premiums if Drug costs needs are low .
- The following is an article that outlines some information about this.
https://thefinancebuff.com/ hmo-ppo-vs-high-deductible-hdhp-hsa.html
- High Deductible plans
- “There is no such thing as a legitimate price for anything in health care,” says George Halvorson
, former chairman of Kaiser Permanente
, the giant health maintenance organization based in California. “Prices are made up depending on who the payer is.”
- "The providers with the most clout are the brand-name medical centers, which hold special cachet for patients and are thus “must have” hospitals for many insurers. “In some markets the prestigious medical institutions can name their price,” says Andrea Caballero, program director for Catalyst for Payment Reform, a national nonprofit trying to get a grip on health costs on behalf of large employers. “They may have brand names of high prestige but not necessarily deliver higher-quality care.”
- Cost shifting by Hospitals – again
- In yet another year of cost increases that exceed Consumer Price Index (CPI) 3+ fold, employers are looking to limit the cost of health benefits by requiring greater employee contributions. (
140-03b
)
- In yet another year of cost increases that exceed Consumer Price Index (CPI) 3+ fold, employers are looking to limit the cost of health benefits by requiring greater employee contributions. (
140-03b
)
- Bottom line: Employers are not able to control the costs of Health Care , because Insurance Companies don't control what care is actually needed (just provide an add-on policies are moot).
- Now that the fiscal irresponsibility
of American Hospital Administration and its self-aggrandizing policies that pretend to control costs is becoming more visible (
Hospitalists
add $200,000 a year each, Nurse Practictioners
cost just as much and more that Primary Care Physicians), the consequences of Vulture Capitalism must kick in. As well, salary inflation of artificially suppressed providers also kicks in.
- Contrast the financial rewards: a Medical Corporation collects a high (40%), Physician earns a low (9%) profit margin
( 140-11 ) 140-11 American Shared Hospital Gross Profit Margin (Quarterly) ( AMS ). pdf <<<OPEN
- Medical Corporation
- Physician Compensation is a small part of Health Care Spending
"Physician compensation accounts for roughly eight percent of the total annual healthcare costs in the U.S., according to Jackson Healthcare, an Atlanta-based healthcare staffing and technology company." (2011)
https://www.jacksonhealthcare.com/media-room/news/ md-salaries-as-percent-of-costs /
- Medical Corporation
- There are Major Issues facing Hospitals
- This article gives a clear discussion of some of the current Hospital ones.
( 140-05 Becker ) 140-05 10 concerns and trends facing hospitals right now.pdf
- Growth of accountable care organizations.
- Huge growth in health IT spending.
- Layoffs
- Competition for physicians.
- Shift from fee-for-service to population health/managed care.
- The growth of high-deductible plans.
- Narrow networks
- Intensity of rivalries.
- Staying independent.
- Reduced inpatient procedures.
- Why Hospitals are losing money (again)
- Forbes (2017)
( 140-12 ) 140-12 Why Major Hospitals Are Losing Money By The Millions | DoctorNews.pdf
- According to the Harvard Business Review, several big-name hospitals reported signifcant
declines and, in some cases net losses to their FY
2016 operating margins
.
Among them, Partners HealthCare
, New England’s largest hospital network, lost $108 million; the Cleveland Clinic witnessed a 71% decline in operating income; and MD Anderson, the nation’s largest cancer center, dropped $266 million. The Cleveland Clinic CEO Dr. Toby Cosgrove
last indicated that 23% of U.S. Hospitals were already in the red in early 2017.
(140-13)
- The problem isn’t declining revenue.
Since 2009, hospitals have accounted for half of the $240 billion spending increase among private U.S. insurers. It’s not that increased competition is driving price wars, either. On the contrary, 1,412 hospitals have merged since 1998, primarily to increase their clout with insurers and raise prices. Nor is it a consequence of people needing less medical care. The prevalence chronic illness continues to escalate, accounting for 75% of U.S. healthcare costs, according to the CDC
.
- Hospitals have contributed to the cost hik
e
in recent decades by:
(1) purchasing redundant, expensive medical equipment and generating excess demand ,
(2) hiring highly paid specialists to perform ever-more complex procedures , rather than right-sizing their work forces
(3) tolerating massive inefficiencies in care delivery.
- A problem is that in the accounting, cutting a Cost (debit) often leads to net revenue loss (asset).
( 5c-01 ) 5c-01 Would Reform Bills Control Costs 2009 HL.pdf- A look to the Agricultural Extension Service.
- A look to the Agricultural Extension Service.
- According to the Harvard Business Review, several big-name hospitals reported signifcant
declines and, in some cases net losses to their FY
2016 operating margins
.
Among them, Partners HealthCare
, New England’s largest hospital network, lost $108 million; the Cleveland Clinic witnessed a 71% decline in operating income; and MD Anderson, the nation’s largest cancer center, dropped $266 million. The Cleveland Clinic CEO Dr. Toby Cosgrove
last indicated that 23% of U.S. Hospitals were already in the red in early 2017.
(140-13)
- HRI
(
Pwc
Health Research Institute - Accounting Services
) projects 2018’s medical cost trend increase at +6.5%
—the first uptick
in growth in three years.
- Administrative Costs
- Ryan Gamlin
presented a report comparing the relationship between health care administrative costs and measures of health system delivery efficiency across ten industrialized countries.
- "As countries spend a larger percentage of their healthcare dollars on administration (as opposed to public health, or providing patient care, for example), things get worse for patients and healthcare providers... I know few physicians at any level of training or practice who believe that administrators are the primary determinant in their ability to deliver safe, effective, and humane care. How then, have we ended up with a top-heavy system, one in which decisions about how care will (or often won’t) be provided are made by those far removed from the experience of caring for patients?"
- Administrative salaries accounted for 22.4 percent of the average hospital's salary costs... Greater enrollment in HMOs, with more competitive bidding by hospitals for managed-care contracts, an important element of proposed managed-competition health care reforms, does not seem to lower hospital administrative costs.
- For example, in his review, Administrative costs were correlated to duplicate lab testing:
admin dupl tests ryan gamlin ( 140-15a ) <<< EXPAND
- "Greater enrollment in HMOs, with more competitive bidding by hospitals for managed-care contracts, an important element of proposed managed-competition health care reforms, does not seem to lower hospital administrative costs."
- Why U.S. hospital administrative costs are among the highest in the world
( 140-18 ) Beckers Hospital CFO Report - 2014
- "
researchers concluded that reforming the U.S. healthcare system to a single-payer model would result in significant administrative savings
. Reducing U.S. administrative spending to the level of Canada or Scotland per capita in 2011 would have saved $158 billion or $156 billion, respectively."
- "
researchers concluded that reforming the U.S. healthcare system to a single-payer model would result in significant administrative savings
. Reducing U.S. administrative spending to the level of Canada or Scotland per capita in 2011 would have saved $158 billion or $156 billion, respectively."
- Health Administrative Cost Improvement
A Comparison Of Hospital Administrative Costs In Eight Nations: US Costs Exceed All Others By Far
( 140-16 ) 140-16 hlthaff .2013.1327. pdf <<< OPEN
- "We found that
administrative costs accounted for 25.3 percent of total US hospital expenditures
—a percentage that is increasing. Next highest were the Netherlands (19.8 percent) and England (15.5 percent), both of which are transitioning to market-oriented payment systems. Scotland and Canada, whose single-payer systems pay hospitals global operating budgets, with separate grants for capital, had the lowest administrative costs." It appears that profit has become the "6th Vital sign in Medicine (after the failed "5th Vial Sign" pain measure that led to the opioid
crisis.
- The belief that having the Hospital systems take over Outpatient settings (Offices) with their high added overhead cost will save money is ludicrous on its face. Hospital Systems have a tremendous marketing advantage, but the excess overhead prevents any overall cost saving. "
Reduction of US administrative costs would best be accomplished through the use of a simpler and less market oriented payment scheme
".
- Higher Administrative Costs are not linked to better-quality care
( 140-16 ) hlthaff .2013.1327. pdf <<< OPEN
administrative healthcare costs.pdf <<< EXPAND
- "We found that
administrative costs accounted for 25.3 percent of total US hospital expenditures
—a percentage that is increasing. Next highest were the Netherlands (19.8 percent) and England (15.5 percent), both of which are transitioning to market-oriented payment systems. Scotland and Canada, whose single-payer systems pay hospitals global operating budgets, with separate grants for capital, had the lowest administrative costs." It appears that profit has become the "6th Vital sign in Medicine (after the failed "5th Vial Sign" pain measure that led to the opioid
crisis.
- Productivity measurement
( 140-17 ) No-Nonsense Guide to Measuring Productivity.pdf (1988)
- "Productivity is not about wages
. High wages can present a problem, not because workers are paid too much but because they produce too little. In deciding how best to measure productivity, managers should focus not on dollars per hour but on labor dollars per product. That is, on labor content, not labor cost.
Workers who are very productive can be paid thousands of dollars more than employees elsewhere and the business can still prosper, as manufacturers like Lincoln Electric have demonstrated"
- Staff specialists and outside consultants
—experts in cost accounting, statistics, and economics—usually play an important role in designing these systems. But these non-medical specialists are "
often trained to focus on the technical elegance and statistical accuracy of productivity indexes.
"
All too often, they introduce methods that are very precise but ignore the real challenges managers face
."
- "Productivity is not about wages
. High wages can present a problem, not because workers are paid too much but because they produce too little. In deciding how best to measure productivity, managers should focus not on dollars per hour but on labor dollars per product. That is, on labor content, not labor cost.
Workers who are very productive can be paid thousands of dollars more than employees elsewhere and the business can still prosper, as manufacturers like Lincoln Electric have demonstrated"
- Ryan Gamlin
presented a report comparing the relationship between health care administrative costs and measures of health system delivery efficiency across ten industrialized countries.
- Health Insurance Excess Costs
- Employer Based Health Insurance
- We as Patients (and even as Medical Workers) often have no idea what Care Costs, where the money comes from or where it goes. Hospitals themselves are a historical money oasis of cost-shifting and poor accounting. The following information is taken from studies by the AHPI
/Kaiser Foundation (2014).
( 13-01 ) 13-01 AHPI _STUDY_Cost_Per_Covered_Life HL.pdf <<<OPEN
( 13-04 ) 13-04 Tax Subsidies for Private Health Insurance.pdf <<<OPEN
"American Health Policy Institute ( AHPI ) is a non-partisan 501(c)(3) think tank, established to examine the impact of health policy on large employers, and to explore and propose policies that will help bolster the ability of large employers to provide quality, affordable health care to employees and their dependents. The Affordable Care Act has catalyzed a national debate about the future of health care in the United States, and AHPI serves to provide thought leadership grounded in the practical experience of America’s largest employers. To learn more, visit americanhealthpolicy.org .
- The average cost of Employer Health Insurance is 30%
of wages. It is 100% Tax deductible.
- We as Patients (and even as Medical Workers) often have no idea what Care Costs, where the money comes from or where it goes. Hospitals themselves are a historical money oasis of cost-shifting and poor accounting. The following information is taken from studies by the AHPI
/Kaiser Foundation (2014).
- Government vs Employment Health Insurance - Taxpayer Subsidy
- Most employed workers do not realize that Employers get Tax breaks for providing their Health Insurance. The rules are complex and varied, but the following illustrates how much more is paid by those who are paid straight wages:
( 13-04 ) 13-04a EmployerHealthWageSavings.pdf <<<EXPAND
- Most employed workers do not realize that Employers get Tax breaks for providing their Health Insurance. The rules are complex and varied, but the following illustrates how much more is paid by those who are paid straight wages:
- Cost per Covered Life Estimations and Taxpayer Subsidy Comparison
The AHPI provided a comparison of Government Insurance with Employment Insurance. They show an average cost of $3,430 per covered life for employer provided coverage and $9,130 per covered life for government provided health care , not including Out-of-Pocket costs to individuals. In other words, government health care spending on a cost per covered life basis is 166 percent higher than private sector employer spending on that same basis.
In general, the Insurance Costs run between $6,000 to $12,000 per covered life per year . Older retired tend to cost more than younger insured, and that contributes to the differences (Medicare - older patients, Employed and Military - younger ones). This explains a great deal of variation in cost, more than the type of insurance coverage.
- Health Coverage Cost Per Covered Life By Funding Source Comparison
- (
13-01
) 13-01aGovernmentvsEmploymentInsurance .
pdf
<<<EXPAND
- (
13-01
) 13-01b1 Costperlife.pdf
<<<EXPAND
- (
13-01
) 13-01aGovernmentvsEmploymentInsurance .
pdf
<<<EXPAND
- Cost Increases have been different for each Insurance Type
( 13-01 ) 13-01c Costperlifechange.pdf <<<EXPAND- Note that Medicaid has had lowest Cost increases.
- Note that Medicaid has had lowest Cost increases.
- National Health Expenditures by type of service and source of funds, CY 1960-2016
[ZIP, 210KB]
These Comparisons tabulated below compare the relative costs of major Health Programs over recent years. Note that medicaid costs have been relatively flat up to the ACA , with increases noted in Medicare and Military/Veterans costs, comparable to Employee insurance increases. ( 130-03 )
- (
13-01
) 13-05 Govt spending by major program.pdf
<<<EXPAND
- 130-03NatExpend.pdf
<<<EXPAND
- (
13-01
) 13-05 Govt spending by major program.pdf
<<<EXPAND
- Private Health Insurance Companies
have become a pass thru for payments, enjoying a high profit for a process they make very complicated and frustrating. Premiums, Co-pays and Deductibles the patient pays is what is tunneled to providers for care. The rest is filtered and retained as Insurance Profit.
- Individual Health Insurance
- Premium costs have increased. A comprehensive policy in 1998 over age 65 was maybe $390 dollars a month. Calculated today this corresponds to $586 monthly. Under age 25 cost would correspond to $262 monthly.
( 148-12 ) 148-04 premiums 1998. pdf
- Co-Pay and Deductible
Obligations - Individuals Employed thru work pay a high Out-of-Pocket.
- Yearly Premium Cost
example for patient with higher
care utilization
(36-0)
36-02b PtCostExample 2016. pdf
- Insurance Company makes a hefty profit despite lower
care utilization
36-01 PtCostExample4 2017. pdf
- As a general rule, Out-Of-Network Providers (HMO or Accepting Assignment) receive 10%
of what the Insurance Organization has collected towards the obligation (named "Allowable Amount"). In-Network Providers receive
20%;
the extra 10% is not for better medical care, however. It is payment for marketing the Health Insurance product. Thus half of the In-Network booty they receive has nothing to do with the care the patient receives - it is an envelope of Cost extorted from the Doctor. Highly marketable and higher demand activties
(such as Robotic Surgeries) may reap up to 40% instead. Take a look at your own Explanation of Benefit statements against this rule-of-thumb). Co-pays and Deductibles generally add up to the payments Providers receive. The rest - pure profit for the Insurance Organization.
- Individual Health Insurance
- Premium costs have increased. A comprehensive policy in 1998 over age 65 was maybe $390 dollars a month. Calculated today this corresponds to $586 monthly. Under age 25 cost would correspond to $262 monthly.
- A reason I suspect patients "like" their coverage from Kaiser HMO plans, for example, is because they don't have to shoulder that 10% extra personal work navigating phone calls and reconciliations of the paperwork themselves rather than the Insurance People (that nice rep you talk to on the phone after waiting maybe 20 minutes to get transferred) and the Computer Screens you and they click thru. The amount of effort and cost savings is dependent on the "Tier" the Services belong to, much as the "tiers" the Pharmacy Drug classification.
- Employer Based Health Insurance
- Practice Costs
- Overhead has been skyrocketing for Physician Offices since 2000. This is an unrecognized factor in health care costs.
- "In the past 15 years, health insurance costs
for employees rose over 200%. Reimbursements
from third-party payers decreased substantially. Technology
has become much more expensive. Documentation
for malpractice purposes has caused physicians to do more paperwork. The billing process
to third-party payers has become much more complicated. Physicians have been forced to hire more staff
. With all of these changes, some physicians have taken a 50% cut in pay – or more
." (
140-03
)
- For example, in 1996, a physician may have had $900,000 in charges. For a reimbursement rate of 60%, he or she would have received $540,000. Deducting total overhead expenses of 44%, or $240,000, leaves his or her salary at $300,000, or 33% of the charges. That same physician in 2011 had charges of $1.4 million. With the reimbursement dropping to 45%, he or she would have received $630,000. Deduct overhead expenses at 68%, or $430,000, and that same physician’s salary has decreased to $200,000, or 14% of his total charges. (140-03)
- "In the past 15 years, health insurance costs
for employees rose over 200%. Reimbursements
from third-party payers decreased substantially. Technology
has become much more expensive. Documentation
for malpractice purposes has caused physicians to do more paperwork. The billing process
to third-party payers has become much more complicated. Physicians have been forced to hire more staff
. With all of these changes, some physicians have taken a 50% cut in pay – or more
." (
140-03
)
- By 2013, overhead for an OBGYN
office had increased to 80%
of revenue
. This happened during a time period of increased Capitation
in reimbursement. Increased staffing that is common in patient-centered medical home models increases the breakeven
capitated
rate. [Capitation appears to have differential effects depending on the specialty/primary care. Perhaps procedure associated specialties may be more cost effect in fee-for-service?]
( 141-02 ) mgma-cost-survey-2014-report-based-on-2013-data-key-finding
( 141-02a ) OperatingCostsToRevenue
- Overhead has been skyrocketing for Physician Offices since 2000. This is an unrecognized factor in health care costs.
- A 2002 survey
outlines how office overhead increased to 60% of revenue in 2002, more since:
( 141-01 ) 141-01a Expense survey- What to spend, what to cut.pdf
- Utilization of Mid-Level Providers in place of Physicians - Cost
- "
In a primary care setting, nurse practitioners may utilize more health care resources than physicians."
- (14-01) 14-01 NP and GP primary care england
- (14-02) 14-03 A Comparison of Resource Utilization HL.pdf
- Belief that replacing FFS
with Managed Care will improve costs has again been proven false. The last time was when the Hospitals went bankrupt in the 1990's. Doing Medicine with selective accounting the first time always costs more.
What avoids waste that is trained Doctors and Nurses having authority. Even NP's are shown to require more cost-cutting; The suggestion is to utilize Medical Assistants to bring down the cost of using Nurse Practitioners.
( 14-02link ) 14-02 New Model txt only annotated.pdf <<<OPENS
-
14-02a NP's need MA's.pdf
<<<EXPAND
- "
In a primary care setting, nurse practitioners may utilize more health care resources than physicians."
- Medicaid Provider Reimbursement (CA, FL)
(155-01) Medicare vs. Medicaid/ Which Pays More.pdf
States reimburse nurse practitioners at anywhere from 75% to 100% of the physician rate. This means that unlike Medicare, some state Medicaid plans treat services provided by nurse practitioners equally to those provided by physicians. In fact, most states reimburse NPs at 100% the rate of MDs.**
151-01a CAreimburses100%.pdf
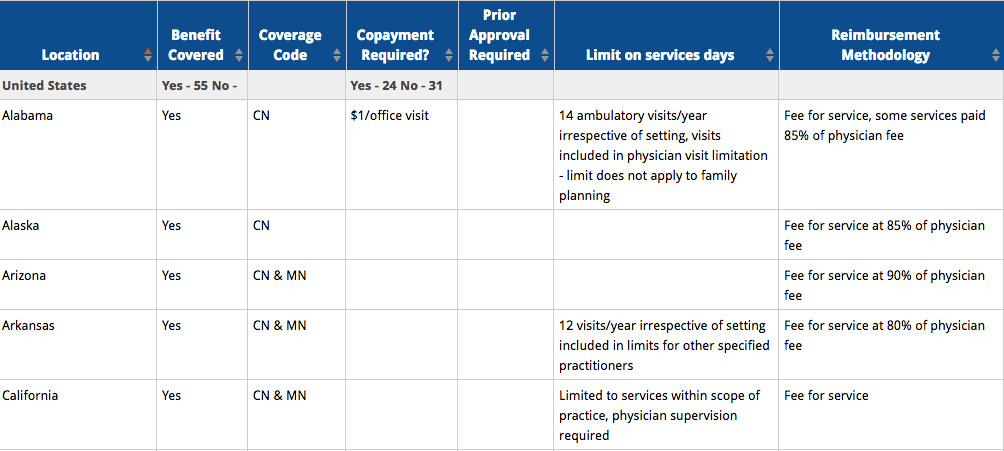
- Medicaid OB Procedure Reimbursement (Missouri)
(152-06) 152-06b medicaid vag.pdf
Vaginal Delivery Procedure Only - What Doctors get paid
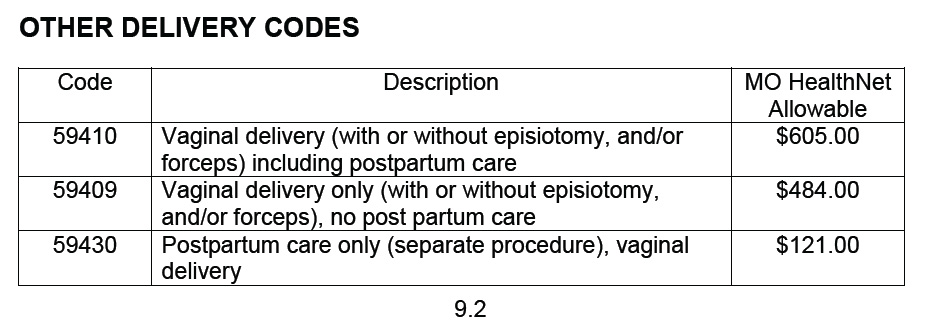
- Medicaid Global OB Reimbursement (Missouri)
(152-06) 152-06a medicaid ob global.pdf
Bundled OB Delivery - What Doctors get paid
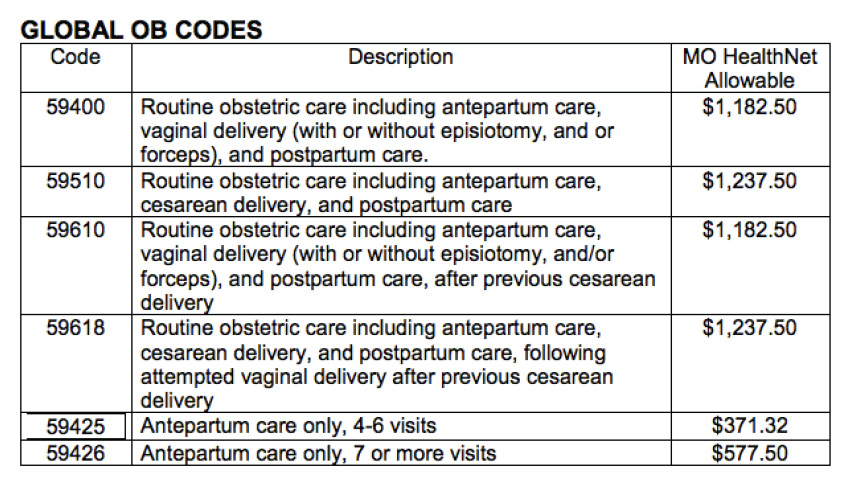
- Florida Physician Medicare Delivery Fee 59400 is higher (2008)
(154-01) FL2007DelFee.pdf
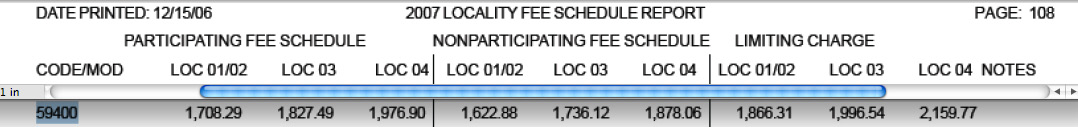
- Proposed changes close small clinics.
(152-03) The future of obsterics, gynaecology and women's health care (2012)
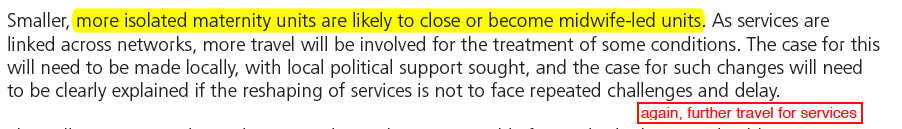
- Annual spending per beneficiary for Medicare has actually been decreasing.
(152-05) Why Has Growth in Spending for Fee-for-Service Medicare Slowed
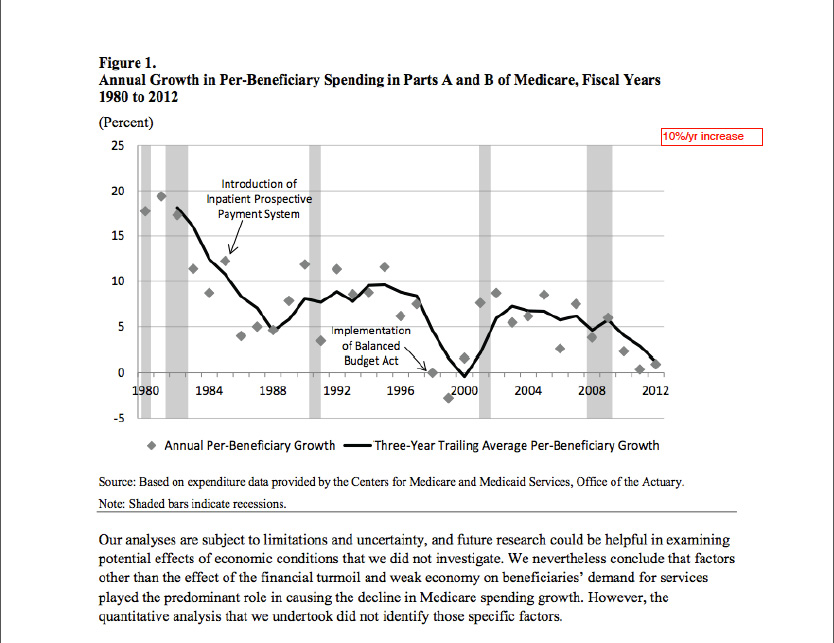
-
(152-05) Medicare Costs Relative to Wages has gone down! (decreased provider reimbursement?).
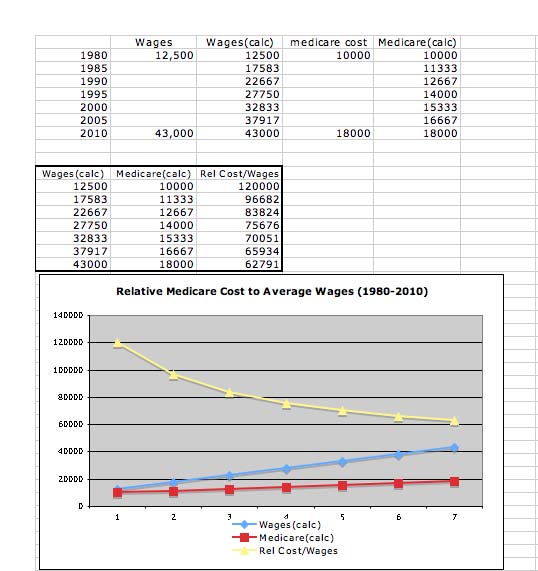
- Hospital Collections from Medicare have been reduced.
(152-04) Typical CA hospital collections
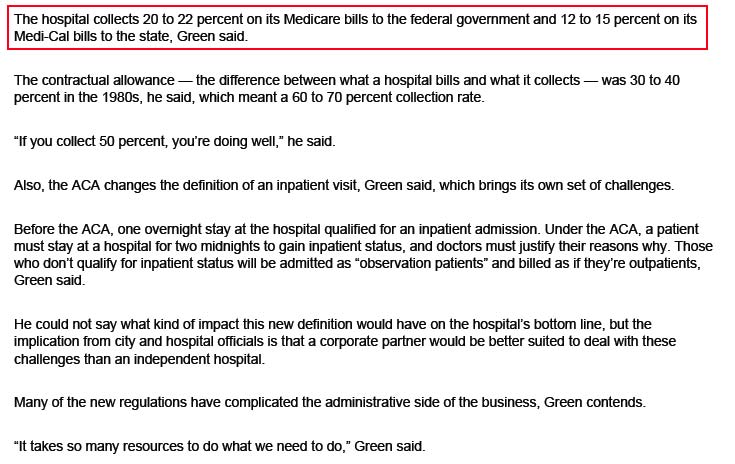
- Medicaid Geographic State Reimbursements
(152-07) From the American College of Nurse Midwives Compensation Survey (a)
Nurse Midwives average a $100,000 salary yearly.
(152-07a) CNM/CM Annual Compensation 2014
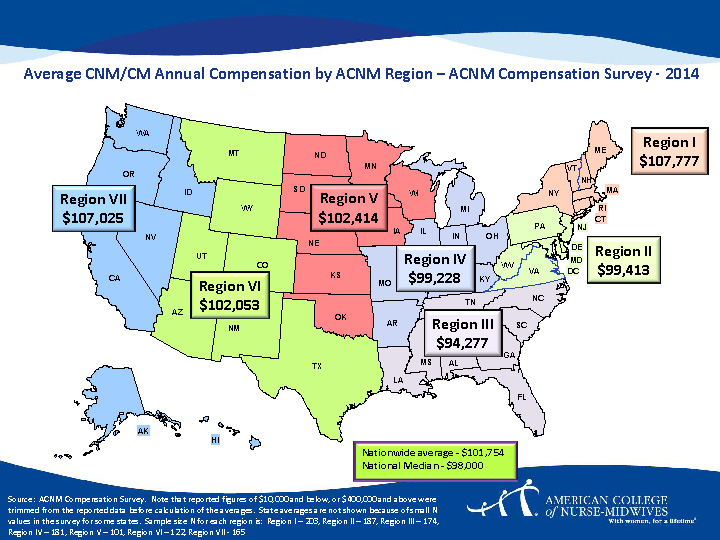
- (152-07b) CNM/CM MEDICAID Reimbursement for Normal Vaginal Delivery
Reimbursement varies by State and Hospital, and Florida Medicaid pays Midwives about 1/2 of those in California, which means the State of Florida subsidizes the use of Midwives in Florida with additional State Tax dollars.
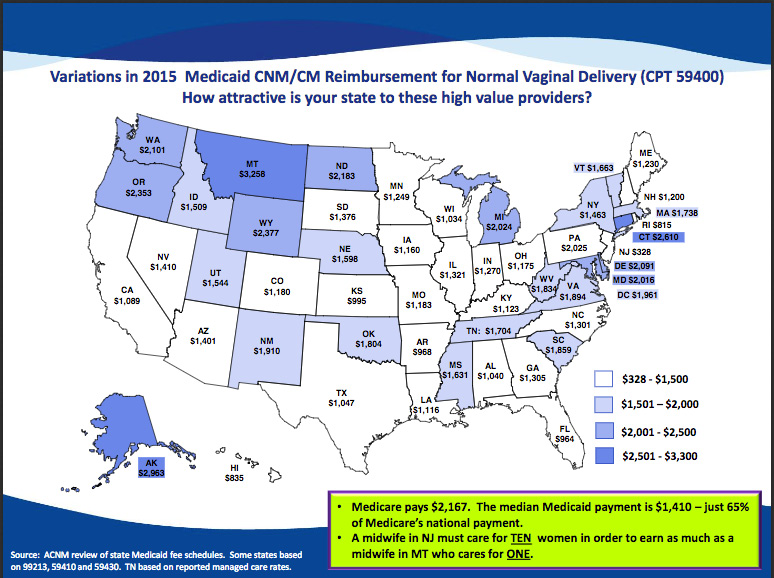
- (152-07d
) CNM/CM get reimbursed 80-100% of Physican Fee.
This is a false potential savings because of the need to provide for acute Physican backup in Obstetrics. As noted above, this affects overall Obstetric costs. That Hospitals were not reimbursing Physicians for this before as the volume increased, and now are either requiring in-house backup coverage or having to pay to obtain this coverage, has led to a spiral of increased Hospital costs. It must also be noted that Nurse Midwives work an average of 38 hours per week, while Physician OBGYN work an average of 55 hours per week.
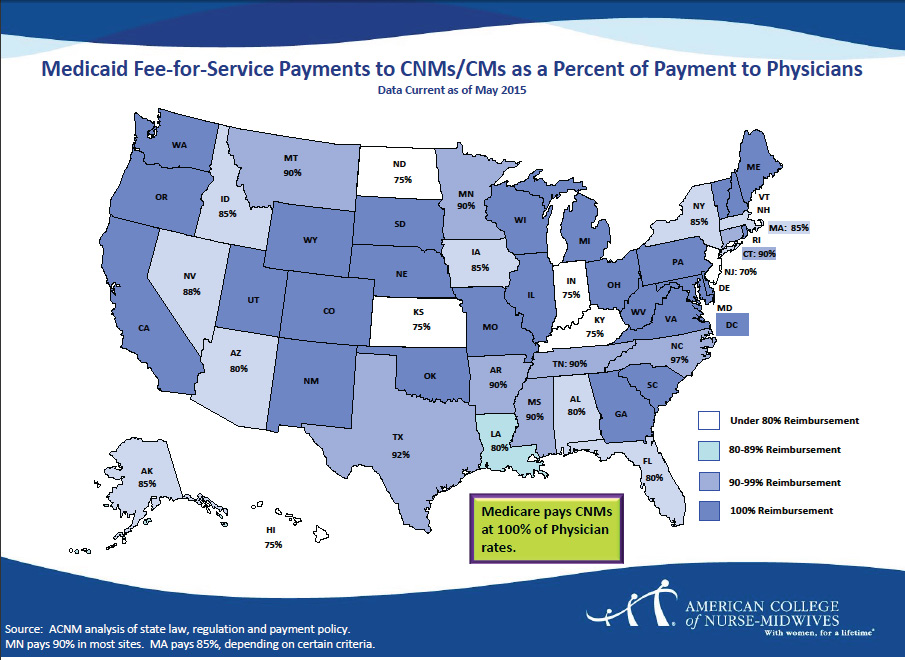
- (152-07c) Physician (MD) Commercial Reimbursement for Vaginal Delivery
Commercial reimbursements are much higher than for Medicaid. Since 50% of deliveries are paid thru Government Medicaid, this indicates a significant underpayment for Medicaid Obstetric services and hence the push to use alternatives to Physicians. Hospitals (and alternative Birthing Centers with lower overhead cost to Commercial Insurance Payers) compete fiercely to get Commercial Insurance patients, who are subsidized by taxpayers at 30-50%.
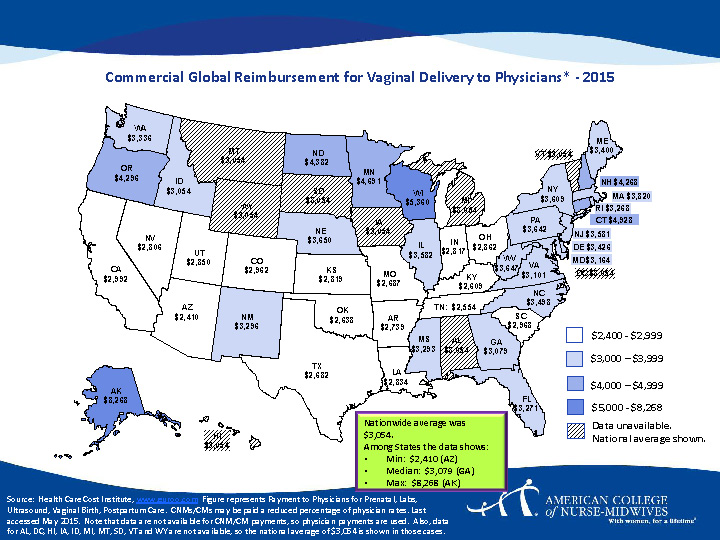
- The Deceptive Salary of Physicians - Cost
Physicians spend about 40,000 hours training and over $300,000 on their education, yet the amount of money they earn per hour is only a few dollars more than a high school teacher. Physicians spend over a decade of potential earning, saving and investing time training and taking on more debt, debt that isn’t tax deductible. When they finish training and finally have an income – they are taxed heavily and must repay their debt with what remains. The cost of tuition, the length of training and the U.S. tax code places physicians into a deceptive financial situation.**
(153-01) 153-01aMDDebtGraphic.pdf
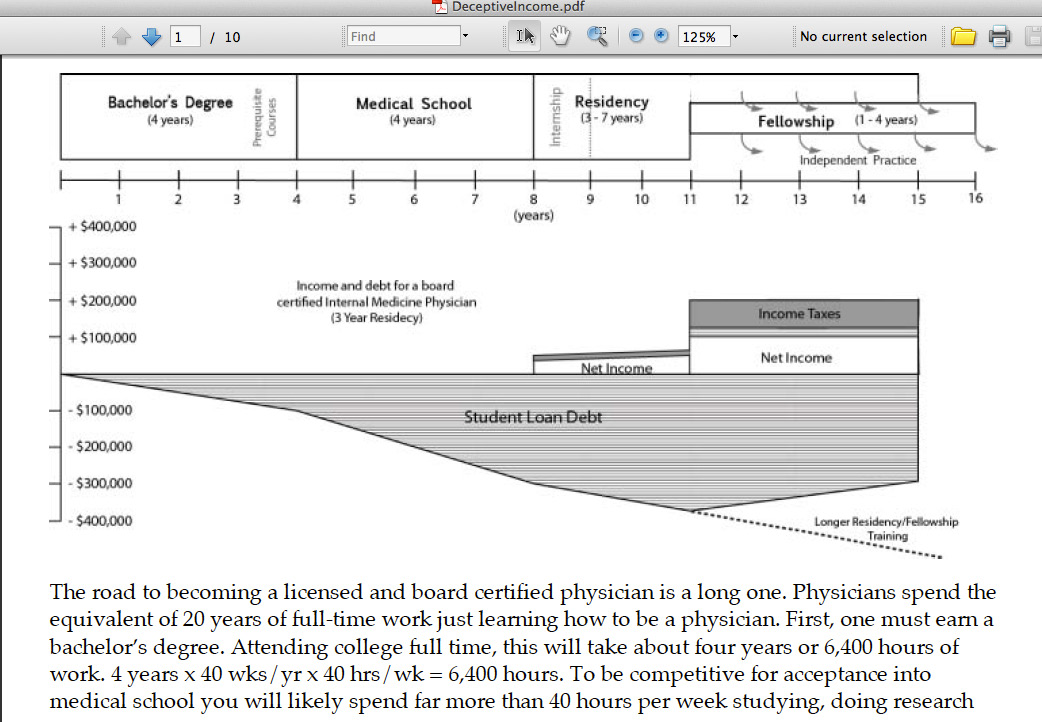
- Royal College of Obstetricians and Gynaecologists in England
(152-03) The future of obstetrics, gynaecology and women’s health care (2012)
- Malpractice Lawsuit Insurance Premiums
- another important problem (not addressed in this report 2/2018)
- The Healthcare Imperative: Lowering Costs and Improving Outcomes: Workshop Series Summary (2010 IOM
)
- The Goal to Standardize Evidence Based Medicine by 2020 (The National Academy of Sciences, Institute of Medicine)
( 171-03 ) 171-03 Bookshelf_NBK53920. pdf <<< OPEN
- The Goal to Standardize Evidence Based Medicine by 2020 (The National Academy of Sciences, Institute of Medicine)
back
- IMPORTANT OVERVIEW REFERENCES
- Summary of CA SB-562 Provisions
- SB562-07.27.2017SUMM.pdf <<< OPEN
- Highlighted CA SB-562 Bill Text (passed 6/2/107; referred to Assembly; tabled)
- SB562-07.27.2017. pdf <<< OPEN
- JP
Massar
- Daily Kos
Explanation of SB-562 Provisions and CNA
Adjuncts (June 7, 2017) (
23-D
)
- 23-D SB-562DailyKos.pdf <<< OPEN Exellent Overview of SB-562
- Senate Health Committee Report - SB-562 based on payroll tax plan (5/14/2017)
(
23-E
)
- 23-E 17.05.14Senate HealthHL.pdf <<< OPEN
- Senate Committee on Appropriations - SB-562 (5/22/2017) ( 23-G )
- Senate Committee on Appropriations - SB-562 Removal of Revenue Planning from Bill (5/25/2017) ( 23-E )
- Senate Floor Analysis - SB-562 ( 23-E )
- Dr. Robert Pollin
, Dr. James Heintz
, Dr. Peter Arno
, Dr. Jeannette Wicks-Lim
(May 2017)
- ( 15-0 ) Pollin-Economic-Analysis-SB -562 HLa.pdf
- Health Care For All - SB-921 Cost and Economic Impact Analysis (2005) (
11-01
)
- Summary of CA SB-562 Provisions
- Healthy California SB-562/CSP2.3 (California Single Payer 2.3)
- There underlying distortion in the public discussion last year. One is that the cost of reform will increase California Resident costs, some stating as much as 3 times the California State Budget.
- General Proposal Universal Health Care - SB-562/CSP2.3 (California Nurses Association)
( 23-H ) Single_Payer_Implications_Employer_Sponsored_Care HL.pdf <<< OPEN
- 23-Ha HealthyCA
Cost.pdf
<<< EXPAND
- 23-Ha HealthyCA
Cost.pdf
<<< EXPAND
- Matt Bruenig
, a widely-read analyst, describes the California Single Payer idea , "currently, government spending on health care in California is around $200 billion and employer spending on health care is between $100 billion and $150 billion... the single-payer plan requires an additional $50 to $100 billion of spending, or 1.9% to 3.8% of CA GDP.... That’s an incredible deal for just 15% of GDP, which again is lower than the United States as a whole already spends on health care"
He adds, "there are challenges to implementing single payer on the state level. States have to deal with all sorts of federal laws like ERISA that could disrupt their plans. States have to hope the federal government will chip in the share they currently contribute to the state’s health-care sector. States have to worry about rich people leaving to avoid tax to some degree. And states have to worry about what will happen during a recession when the state’s budget contracts in ways the federal government’s budget does not. But if the plan would work like this report says it does and at the cost this report says it does, it is a no-brainer ." (151-01)
( 151-01 ) 151-01 California Single Payer Is a No-Brainer . pdf <<<OPEN
- There underlying distortion in the public discussion last year. One is that the cost of reform will increase California Resident costs, some stating as much as 3 times the California State Budget.
- Dr. Robert Pollin
, Dr. James Heintz
, Dr. Peter Arno
, Dr. Jeannette Wicks-Lim
(May 2017)
******( 15-0 ) Pollin-Economic-Analysis-SB -562 HLa.pdf ***** <<<OPEN
This extensive analysis was sponsored by the California Nurses Assn./National Nurses United
- Media articles and discussions this year about SB-562 have focused on the CA Senate Appropriations Committee Report (May 4, 2017) without seriously looking at the additional University of Massachusetts Amherst Pollin
Report. This was released just days before the Bill passed in the Senate and immediately tabled in the Assembly (June 1, 2017). It is an exhausting look at the major provisions of the CSP
2.3 Plan advocated by the California Nurses Association.
- "Working from the weight of evidence from the relevant research literature, it is reasonable to conclude that a single-payer system in California will generate substantial cost savings in a range of areas relative to the state’s existing system."
- "The study finds that the providing full universal coverage would increase overall system costs by about 10 percent, but that the single payer system could produce savings of about 18 percent. The study thus finds that the proposed single-payer system could provide decent health care for all California residents while still reducing net overall costs by about 8 percent relative to the existing system. We propose two new taxes to generate the revenue required to offset the loss of private insurance spending: a gross receipts tax of 2.3 percent and a sales tax of 2.3 percent, along with exemptions and tax credits for small business owners and low-income families to promote tax-burden equity."
- "The study finds that the providing full universal coverage would increase overall system costs by about 10 percent, but that the single payer system could produce savings of about 18 percent. The study thus finds that the proposed single-payer system could provide decent health care for all California residents while still reducing net overall costs by about 8 percent relative to the existing system. We propose two new taxes to generate the revenue required to offset the loss of private insurance spending: a gross receipts tax of 2.3 percent and a sales tax of 2.3 percent, along with exemptions and tax credits for small business owners and low-income families to promote tax-burden equity."
- California Current State Health Expenditures
currently is $370 billion
(14% of California GDP 2017).
- California State provides 9% of Care in subsidies.
- The net costs of health care under the present system range between 3.4 and 9.9 percent of a families’ income.
- Medicare (retirees) and MediCal
(lo-income) provide additionally half of all health care funding in California. The State must obtain waivers so that present funding sources will continue to finance Healthy California ($225 billion of ). This is one area of concern.
- By contrast, California’s high-income families are presently receiving a net subsidy of 1 percent of their income
to support their own health care coverage.
- California State provides 9% of Care in subsidies.
- Uninsured/Underinsured Californians
- 92% of Californians have some form of Health Insurance
coverage.
36% of the insured have high deductibles
and/or large out-of-pocket expenses.
( 15-0 ) 15-0a Pollin-Economic Insurance Coverage ref.pdf <<<EXPAND
- 23 percent
of insured individuals in the United States had sufficiently high deductibles or other out-of-pocket costs to be considered underinsured
. 19 percent of California residents would be considered underinsured because of high deductibles and out-of-pocket expenses
. according to the Commonwealth Fund Biennial Health Insurance Survey in 2014.
- For the U.S. overall, the average uninsured
person had half the amount of medical expenses as the average insured person ($2,443 versus $4,876)
, according to an extensive 2014 study by Coughlin
et al., "Uncompensated Care for the Uninsured in 2013".They paid out of pocket an additional $25.8 billion for their care
.
- The
cost to providers of uncompensated care was $84.9 billion
, with 60 percent of this care being provided by hospitals, with clinics, health care centers and office-based physicians providing the remaining uncompensated care (40 percent).
- The Healthy California (
CNA
) proposal would eliminate all forms of cost-sharing, including all deductibles, co-payments and other out-of-pocket expenses
.
- 92% of Californians have some form of Health Insurance
coverage.
36% of the insured have high deductibles
and/or large out-of-pocket expenses.
- Expanding coverage to Universal Health Care (without Single payer) is estimated at $404 billion
(added +10% more) under the current system. 110-04 table 6.
pdf
- Single Payer Health care for all California residents can reduce net overall business costs by (-18%)
,
while promoting tax-burden equity (CSP2.3).
- CSP2.3 Areas of Expected Savings (-13%
)
- Savings in Administration
- Private insurance administration and profits, which accounts for $15.8 billion, or ( 50 percent) of this category
- The other large share of spending in this category is for public administration of Medicare and MediCal programs. These account for $12.4 billion in spending for 2017, or nearly (40 percent) of spending in this overall administrative category.
- Public health activity amounts to $9.0 billion in total health care spending in California (
10 percent
).
- Savings in Drug Pricing
- "We conclude that the cost savings potential in the area of pharmaceutical pricing within Healthy California should be at least 30 percent. In fact, additional evidence with respect to current trends in the U.S. pharmaceutical market reinforces our conclusion that this 30 percent cost-reduction figure is a lower-end figure."
- "We conclude that the cost savings potential in the area of pharmaceutical pricing within Healthy California should be at least 30 percent. In fact, additional evidence with respect to current trends in the U.S. pharmaceutical market reinforces our conclusion that this 30 percent cost-reduction figure is a lower-end figure."
- Savings from a Set Fee Schedule
- Small Firms enjoy a -22% decrease in business cost
- Medium Firms see a -13to-7% decrease cost
- Large Firms up to 500 Employees have a -5.7% decrease cost
- Largest Firms over 500 employees have a -0.6% decrease
cost
- Savings in Administration
- Areas of Overhead Waste Saving
s (
-5%, 1/4 of the 19% of the IOM
estimated current overspending
)
- unnecessary services
- inefficient delivery
- lack of prevention
- fraud
- Estimated HealthCare
Waste (2011)
175-01 Waste Category Estimate 2013 Scripps Quality Summit . pdf
- Estimated HealthCare
Waste (2009)
( 173-01 ) 173-01a USHealthcare Waste.pdf <<< EXPAND
- While a broad consensus exists in the research literature as to the rough magnitude of overspending in the areas of service delivery, there is much less agreement as to how much cost savings can be realistically achieved through any given set of reforms in care delivery.
- Hospital owned practices cost more
- With respect to California specifically, Schulman and Richman
report that, for 2012, costs of care per patient were about
56 percent higher
when the patients were seen in a physician practice owned by a multihospital system as opposed to a practice owned independently by a physician.
- With respect to California specifically, Schulman and Richman
report that, for 2012, costs of care per patient were about
56 percent higher
when the patients were seen in a physician practice owned by a multihospital system as opposed to a practice owned independently by a physician.
- Kaiser HMO
- At the same time, because Kaiser is already covering about one-fourth of the state’s insured residents on the basis of a relatively efficient delivery system, the additional potential gains in efficiency that are available in California are likely to be less than the lower-bound 18.8 percent figure established by the IOM
for the U.S. overall.
- At the same time, because Kaiser is already covering about one-fourth of the state’s insured residents on the basis of a relatively efficient delivery system, the additional potential gains in efficiency that are available in California are likely to be less than the lower-bound 18.8 percent figure established by the IOM
for the U.S. overall.
- Hospital owned practices cost more
- Achieving significant improvements in the areas of service delivery will also be critical for controlling the longer-term pattern of cost and price increases over time. The structural changes that we have examined—in the areas of administration, pharmaceutical pricing and hospital, physicians/clinics and dental fees—are capable of generating significant one-time cost reductions as well as establishing an improved overall framework for controlling costs over time. But it is still the case that, even with a dramatically restructured health delivery system through Healthy California, costs can continue to rise excessively through ineffective delivery systems.
- Change in health care utilization is a theoretical concern with decreased Co-Pays, but experience shows this does not materialize
.
- CSP2.3 Areas of Expected Savings (-13%
)
- Media articles and discussions this year about SB-562 have focused on the CA Senate Appropriations Committee Report (May 4, 2017) without seriously looking at the additional University of Massachusetts Amherst Pollin
Report. This was released just days before the Bill passed in the Senate and immediately tabled in the Assembly (June 1, 2017). It is an exhausting look at the major provisions of the CSP
2.3 Plan advocated by the California Nurses Association.
- CSP2.3 CNA
supported Funding Proposal
(
"2.3 - Nothing is Free"
)
- Two universal taxes are proposed in the California Nurses Plan, set at the rates and under the specific provisions stipulated, to raise the additional $106 billion
, to allow the planned Expanded and Universal coverage from the Cost Savings. This has been analyzed in the Pollin
Report (May 2017)
- A gross receipts tax of 2.3 percent.
(Wholesale Business Tax on over $2million gross)
This tax will be applied to all businesses in California. It will include an exemption for the first $2 million in receipts for all businesses. Through this exemption, firms that average up to 9 employees will have no gross receipts tax obligation. Firms with up to 19 employees will pay taxes on only about one-third of their gross revenue. Representative firms of all sizes wil be at least no worse off through Healthy California relative to conditions with the existing system. In most cases, the firms be significantly better off.
- A sales tax of 2.3 percent
(on non-essentials)
The sales tax will exempt all spending on housing, utility and food at home. To be consistent with the existing California tax code, it will also include exemptions on a broad range of service expenditures. It further includes a 2 percent income tax credit for families currently insured through MediCal , to fully offset their 2.3 percent sales tax spending.
- A gross receipts tax of 2.3 percent.
(Wholesale Business Tax on over $2million gross)
- Two universal taxes are proposed in the California Nurses Plan, set at the rates and under the specific provisions stipulated, to raise the additional $106 billion
, to allow the planned Expanded and Universal coverage from the Cost Savings. This has been analyzed in the Pollin
Report (May 2017)
- Limitations of the Pollin
Analysis
- Does not analyze the full range of economic effects of Healthy California.
- Does not undertake a dynamic analysis of the change in California’s health care system on private investment and employment due to decreased health care costs for firms that are presently providing coverage for their employees.
- Does not examine how overall household consumption behavior may change from health care costs falling for low- and especially middle- income families, while rising modestly for high-income families.
- Does not address the major challenges that the California economy will face as it proceeds with the transition out of the existing health care system . Maryland's experience may inform this.
- Each of these important issues, as well as other related matters of significance, are reported to be in examination by the proponents of SB-562, but not been given the opportunity for examination.
back
- CSP2.3 moves Federal Medicare Parts A, B, and D supplemental costs into a State Sales Tax
. Patients can also buy insurance for extra benefits not covered.
-
CSP2.3 retains none of the network restrictions found in Standard Medicare -patients can go to any participating provider with no premiums, no co-pays and no deductibles.
-
CSP2.3 contracts directly with providers as negotiated Fee For Service.
-
CSP2.3 reduces the Tax, Employer and Third-Party controls for Medical Care, but widens the Risk Base.
-
CSP2.3 is closer to the source, with more transparent overhead. It allows for enrollees to purchase additional insurance for uncovered services. Local utilization review is shown to be necessary, even for Medicare.
back
- The SB562 approach is not perfect and has some pain. Many alternative provisions that would be helpful depending what is the goal. However, the HSC
Committee feels the evidence supports Single Payer, Universal Health Care, and at the State Level.
-
It covers all California Residents under the age of 65 regardless of governmental status
-
Workmen's Compensation coverage is included for the first year
-
It corrects the error that has been repeated of assuming Capitation will control costs. It does not, and makes all services Fee-for-Service.
-
It corrects the error of requiring Electronic Health Records Systems of Physicians which has added 20%to Office Overhead, and 10-20% deceased productivity in Medical offices across the Board.
- On balance there are so many of the issues about providing a stable Medical Program for Residents of the
State, that it is unwise to pass up the opportunity.
back
-
There are some other State attempts, more interest being generated. The State that has demonstrated the most activity towards Single Payer Health Care is Maryland.
-
State Single Payer Legislation Information by State
( 149-23 ) 149-23 State Single Payer Legislation.pdf
Single payer advocacy groups in many states are successfully pursuing state-level legislation. This legislation is a constantly moving target.
-
Vermont
Single Payer Program
-
Vermont Single Payer Architect accused of violating the civil False Claims Act.
- Jonathan Gruber , PhD, is a professor at Cambridge-based Massachusetts Institute of Technology and known as a chief architect of the Affordable Care Act.
- Dr Gruber won a state contract in 2014 to conduct economic modeling for Vermont's proposed single-payer health care system.
- The Vermont Attorney General's Office concluded Dr. Gruber violated the civil False Claims Act by allegedly submitting false invoices to the state.
- In November 2014, a video surfaced of Gruber saying that the Affordable Care Act passed because of "the stupidity of the American voter." Vermont changed Gruber's contract so that only his research assistants would be paid for the remainder of the work.
- Dr. Gruber
denied the claim. However, in the settlement he agreed to release his claim to both the $40,000 outstanding payment and the $50,000 for his research assistants, according to the report.
-
Vermont Single Payer Architect accused of violating the civil False Claims Act.
-
Texas
- Texas has fewer health insurance regulations than most states... Health insurance laws in some states strictly regulate the cost and availability of health insurance policies, instead of letting insurance companies have complete freedom. Texas health insurance laws are rather relaxed
in this area, which means you have to be more aware of what liberties your Texas health insurance company are allowed. (148-11)
- Texas has fewer health insurance regulations than most states... Health insurance laws in some states strictly regulate the cost and availability of health insurance policies, instead of letting insurance companies have complete freedom. Texas health insurance laws are rather relaxed
in this area, which means you have to be more aware of what liberties your Texas health insurance company are allowed. (148-11)
-
Maryland
-
See discussion ahead.
-
See discussion ahead.
-
State Single Payer Legislation Information by State
back
back
-
Survey of other States that have utilized Gross Business Taxes (Receipt or Excise Taxes):
-
Alabama-
- Alabama has a Gross Receipts Tax on utilities only.
-
Arizona-
- Transaction Privilege Tax (Gross Tax) is collected on various business activities, ranging under 3% .
- Arizona's also collects tax on taxable income (6.9% corporate rate now reduced to 4.9% .)
-
Delaware-
- Delaware's Gross Receipts Tax is a tax on the total gross revenues of a business, regardless of their source. This tax is levied on the seller of goods or services, rather than on the consumer. Business and occupational gross receipts tax rates range from 0.096% to 1.92%, depending on the business activity. There are no deductions for the cost of goods or property sold, labor costs, interest expense, discount paid, delivery costs, state or federal taxes, or any other expenses allowed. (110-01)
- Delaware combines this with an additional Corporate Business Tax .
-
Florida-
- Florida has a 2.5% Gross Receipts Tax on Utilities.
-
Hawaii-
- Hawaii imposes a General Excise Tax (GET) as a Gross Receipts Tax
on all business done in Hawaii, at 0.5% for wholesaling and manufacturing, 0.15% for insurance commissions, and 4% (4.5% in Honolulu county) for all other activities. Businesses may pass on the GET as a sales-tax-like surcharge but are not required to do so.
- Hawaii imposes a General Excise Tax (GET) as a Gross Receipts Tax
on all business done in Hawaii, at 0.5% for wholesaling and manufacturing, 0.15% for insurance commissions, and 4% (4.5% in Honolulu county) for all other activities. Businesses may pass on the GET as a sales-tax-like surcharge but are not required to do so.
-
Nevada-
- Nevada has a notable Gross Receipts Tax combined with a
Modified Business Tax
that has evolved.
-
Commerce Tax
https://taxfoundation.org/ nevada-approves-commerce-tax-new-tax-business-gross-receipts
v-
The
"
Commerce Tax
"
is a modified
Gross Receipts Tax. It divides Nevada’s economy into 26 business categories, each assigned its own gross receipts tax rate, with rates ranging from
0.051 percent to 0.331 percent
. Businesses which do not fit into any other category are taxed at th
e 0.128 percent rate for Unclassified Businesses.
- The Commerce Tax is levied on a businesses’ Nevada gross revenue in excess of $4 million per year
(less certain subtractions
including distributions from pass-through entities, stock proceeds, bad debts expensed on federal taxes, and net income from a passive entity to the extent that income was generated by another business entity). It is modeled after the Gross Receipts Taxes in Ohio, Texas, and Washington States. Sectors already paying gross receipts taxes (gaming, mining, and insurance) exclude from the Commerce Tax any revenue subject to those taxes.
-
The gross revenue of a business entity is determined by taking the total amount from engaging in a business in this State with no deduction for cost of goods sold or other expenses incurred in operating the business. (Section 8(2), 8(3) of Senate Bill 483) (129-02,04)
-
While the Commerce Tax is not identical to earlier gross receipts tax proposals (including those rejected by legislators in 2003 and rejected by voters in 2014), it is still a Gross Receipts Tax and "retains the flaws inherent to such a tax." These had fallen out of favor since their peak popularity in the 1930s because of arguments about the pyramiding and non-neutrality inherent within their structure.
-
In an acknowledgement that different industries experience vastly different average profit margins, the Commerce Tax divides the state’s economy into 26 categories, each with its own tax rate. There is little reason to think that these rates, based on a one-year study of Texas’s economy, are an accurate reflection of comparative profit margins across industries in Nevada. However, even if they captured comparative margins perfectly in the aggregate, they can never be sufficiently granular to reflect the actual experience of any particular company.
- The retail sector, by way of example, is subject to a 0.111 percent tax on gross receipts under the Commerce Tax. "Even if this rate were a perfect expression of the relative profit margins of the retail industry within the broader economy, the profit margins of subsectors
could vary dramatically."
-
The
"
Commerce Tax
"
is a modified
Gross Receipts Tax. It divides Nevada’s economy into 26 business categories, each assigned its own gross receipts tax rate, with rates ranging from
0.051 percent to 0.331 percent
. Businesses which do not fit into any other category are taxed at th
e 0.128 percent rate for Unclassified Businesses.
-
Modified Business Tax
- Nevada Revised Statutes 363B.120 provides an abatement of the Modified Business Tax for qualifying businesses. The business tax is imposed on each employer at the rate of 1.17% on taxable wages over $85,000 in a quarter. Tax is based on gross wages paid by the employer
during a calendar quarter. Employers may deduct allowable health care expenses from the taxable wage amount. A business approved pursuant to NRS
360.750 can receive a partial abatement of up to 50 percent of the amount of the business tax due during the first four years of operations.
-
Tax rates are derived from a 2011 study of the Texas Margin Tax which attempted to calculate the effective tax rates experienced by firms across a range of industry classifications. Rates on food services, retail, and wholesale were doubled to adjust for half-rates imposed on those sectors in the Texas plan. The accommodations tax rate was adjusted upward, and the telecommunication tax rate was combined with utilities and thus taxed at a lower rate, a concession to what is likely the first of many lobbying efforts to alter an industry’s category or rate.
- Nevada Revised Statutes 363B.120 provides an abatement of the Modified Business Tax for qualifying businesses. The business tax is imposed on each employer at the rate of 1.17% on taxable wages over $85,000 in a quarter. Tax is based on gross wages paid by the employer
during a calendar quarter. Employers may deduct allowable health care expenses from the taxable wage amount. A business approved pursuant to NRS
360.750 can receive a partial abatement of up to 50 percent of the amount of the business tax due during the first four years of operations.
-
Commerce Tax
-
After the first year of the Commerce Tax, a partial credit was offered against the Modified Business Tax (
MBT
) liability, limiting the degree to which businesses are subject to taxes by the two different liabilites
. By reducing MBT
rates as state revenue grows and crediting Commerce Tax payments against MBT
liability, the Commerce Tax’s total share of business tax revenue increased over time.
-
The difference between a Sales Tax and a Receipts Tax is which cost or value serves as the basis and who pays it. A $100 radio with a 10% Sales Tax costs the customer $110. $100 goes to the Business, $10 to Tax. 10/110 = 9% (percent of total cost to consumer), 10/100 = 10% (percent of item cost). If the profit is $50, then that is 50/110 = 45% of total cost, 15/100 = 15% of retail cost. Taxing the profit at 33% is a gross tax cost of $5. Taxing the gross at 5% is a tax of $5 (but tax is hidden in the acquisition costs of the business). To the customer, tax and retail cost are indistinguishable. To the business the tax costs are mixed with overhead costs. An additional problem is no balance sheet entry for time variable asset and liabilities.
-
Some Industries are more profitable than others. Why is it ok to give tax breaks to carried interest investors and real estate arbitragers instead of workers. These can be adjusted.
-
Which is the more appropriate to tax? Would a breathing tax be useful? People who exercise more use a higher share of the available oxygen in the atmosphere, so should get a mask metering their use of air and pay accordingly. How about child lemonade stands? Do we monetize every asset and paralyze those which have no monetization?
- Nevada has a notable Gross Receipts Tax combined with a
Modified Business Tax
that has evolved.
-
New Mexico-
- The gross receipts tax rate varies throughout the state from 5.125% to 8.6875% with local option taxes imposed at the city and county levels, added to the statewide base tax rate of 5%. Items include selling, leasing or licensing property, granting a right to use a franchise, performing services, and selling research and development services.
-
Some deductions are allowed for out-of-state sales.
-
Ohio-
- The Commercial Activity Tax
(CAT) is levied on Businesses with annual taxable gross receipts
in excess of $1 million. they pay the annual minimum tax plus the product of a tax rate of 0.26% after subtracting the exclusion amounts (
basically taxable gross receipts includes sales of property (including intellectual property), performance of services, and rent
. Each taxpayer may exclude the first $1 million of taxable gross receipts for a calendar year.
- The Commercial Activity Tax
(CAT) is levied on Businesses with annual taxable gross receipts
in excess of $1 million. they pay the annual minimum tax plus the product of a tax rate of 0.26% after subtracting the exclusion amounts (
basically taxable gross receipts includes sales of property (including intellectual property), performance of services, and rent
. Each taxpayer may exclude the first $1 million of taxable gross receipts for a calendar year.
-
Pennsylvania- (161-01)
- A Gross Business Tax of about 0.05% is levied on some Industries: pipeline, conduit, steamboat, canal, slack water navigation, and transportation companies; telephone, telegraph, and mobile telecommunications companies; electric light, water power, and hydroelectric companies; express companies; palace car and sleeping car companies; and freight and oil transportation companies.
- Corporate Net Income Tax is 9.9% for most applicable industries as well.
-
Tennessee-
-
A
Gross Receipts Tax
is imposed on certain Industries: Bottlers, Utilities – Gas, Water, Electric, Vending, Mixing Bar Companies
-
A
Gross Receipts Tax
is imposed on certain Industries: Bottlers, Utilities – Gas, Water, Electric, Vending, Mixing Bar Companies
-
Texas-
-
Gross Receipts Tax
on Utilities 0.6% to 2%.
-
Gross Receipts Tax
on Utilities 0.6% to 2%.
-
Virginia-
-
Gross Receipts Tax
with a Corporate Business Tax and Retail Sales tax
-
Gross Receipts Tax
with a Corporate Business Tax and Retail Sales tax
-
Washington State-
-
Gross Income Tax
(
"Business and Occupational Tax"
)
- Gross income is "income earned by the business for products sold or services rendered," including retail sales. "There are no deductions allowed for costs of doing business, materials used, labor or delivery expenses, or taxes." ( 129-01 ) 129-01 What is a State Gross Receipts Tax_. pdf
-
Wikipedia
cites the following comments about Washington's Gross Receipts Ta
- "Economists have criticized gross receipts taxes for encouraging vertical integration among companies and imposing different effective tax rates across different industries."
- The source of this quote is Andrew Chamberlain from a 2006
psoting
on the
TaxFoundation.org
website.
( 117-02 ) 117-02 tax pyramiding sr147. pdf <<< OPEN
See Paul Krugman's comments about the reliability of the Tax Foundation ahead.)
- Most Washington businesses fall under the 1.5% gross receipts tax rate, manufacturing, wholesaling and retailing are 0.5%
-
There are no deductions for business expenses, except for income from a different state. Also, if you have a small business, there is a tax credit for you—one of the best things about Washington State taxes.
-
Sales tax.
The Washington sales tax you must charge, collect, and pay the state depends on what county you’re in. The interesting part of this is, because Washington has an income tax on your gross receipts, they will always know what your gross sales are, and thus, automatically calculate the sales tax that you should have collected and owe the state. So, if you screw up and don’t collect the right amount of tax, you still will owe the right amount to Washington.
The base Washington state sales tax rate is 6.5, and each location (county or city) charges a local rate on top of that. So, for instance, in Issaquah , total sales tax is 9.5%, but in Pomeroy it’s 7.5%
-
Use tax
is a tax law written to tax the heck out of everyone. Let’s say you buy a desk at a garage sale for your office. Technically you should have to pay sales tax for that, but no garage sale person or Craigslist
seller is going to charge you sales tax. So, Washington has a law called use tax, governed under Chapter 82.12 of the Revised Code of Washington.
In theory, if you bought a desk for $100 at a garage sale, you should report that and pay use tax because you couldn’t pay sales tax.
Another loophole the use tax aims to close is out-of-state purchases. Say someone buys a $750,000 excavator in Oregon or Montana where there’s no sales tax and brings it into Washington State to work with it. If they get caught with it in Washington State, the Department of Revenue will charge that person or business use tax.
-
Use Tax Rates in Washington
The use tax is always going to be the same as the sales tax in your local area. While the sales tax rate is determined by where you buy something, the use tax is determined by the sales tax rate where you first use it.
Use tax affects individuals also. If a Washington resident went to Portland to buy school supplies or make a big purchase and bring it back to their home in Washington, they are supposed to report that personally to the Washington Department of Revenue and pay sales tax on that.
-
Use Tax Rates in Washington
-
Property tax
The Washington State personal property tax is a true double tax by every definition. Again, say you pay sales tax to buy a desk for your office. You’ll first pay sales or use tax, and then business personal property tax every year you own it. Isn’t there just something wrong about business personal property tax? Personal Property is taxed on the current market value of all assets used for business
-
Income tax
. Washington has the 11th best business tax climate in the country, according to the Tax Foundation. The good news about Washington taxes is that there is no actual income tax
. There is, however, a business and occupation (B & O) tax, sales tax, and use tax that affect most businesses in Washington State. Let the following be your guide to understanding Washington business taxes. (
129-07
) 129-07 How Washington State Business Taxes work - WA B&O Tax.pdf
-
Gross Income Tax
(
"Business and Occupational Tax"
)
-
Alabama-
-
Additional discussion about the viability of Gross Taxes in States (from Tax Foundation Reports***)
-
According to the Tax Foundation article, "In the past ten years, four states that had utilized Gross Receipts Tax eliminated them. As outlined here, this has been part of the ebb and flow largely determined by Legislature mistakes and shortfalls in their Budgets:
- Michigan - did not have a Gross Receipts Tax
- Indiana - has instituted massive other taxpayer taxes.
- Kentucky
-
New Jersey
-
Indiana
- Indiana completed a four-year phase down of its corporate income tax rate from 8.5 to 6.5 percent, the culmination of legislation adopted in 2011. Subsequent legislation enacted in 2014 established a further schedule of rate reductions through fiscal year 2022, when the corporate income tax will drop to 4.9 percent. For 2017, the rate declined from 6.5 to 6.25 percent, which, along with the elimination of the state’s throwback rule, bumped the state’s corporate component rank from 24th to 23rd. The state ranks 8th overall, an improvement
- Indiana has now assuemed a high level of debt to fund their programs.
- Indiana greatly increased its Gas Taxes.
-
Indiana has a high level of private prisons who pay diminished taxes.
-
Michigan
- I commend (article 123-01) to our CA State Legislators
the excellent interesting exploration about the rationale for Business taxation in their adoption of its S
ingle Business Tax
(
SBT
, a Value Added Tax, and its history of the ping-pong taxation experiments in Michigan from 1946 to 2003 and beyond. Michigan has a storied history dealing with Health Care worth examining.
- It seems that strangely California has been following in Michigan's historical footsteps in that regard. This should be a wakeup
regarding the Assembly's deplorable inaction relating to SB-562. It seems to revert to backroom discussions about the "distribution of business tax liability" instead of clear headed examination of the options.
-
However, Michigan has not actually used a Gross Receipts Tax, although it has used Value added taxes based on gross receipts deducting expenses and taxes at each step.
123-01 Background and History_ Michigan's Single Business Tax.pdf
-
Three classes of percentage Business Taxes
are identified: (122-03)
-
Net Income/Profits Based Tax
Net income or profits-based taxes, which are levied in 44 states, are equal to total revenue less business expenses or total costs. Deductible business expenses include such items as cost of materials, labor, interest, rent, and depreciation. The principal argument for corporate income taxes, as opposed to other business taxes, centers around the idea that only businesses that make a profit should have to pay a business tax.
-
Gross Receipts Tax
Gross receipts taxes, which are levied in only a few states, are based on gross receipts, total revenue, or gross volume of sales. Gross receipts taxes make no adjustment for or subtraction of the cost of materials used. Because materials produced by one business may be purchased for use by another business, the amount of tax tends to be compounded (i.e., the potential exists for the same item/purchase to be taxed multiple times) in this type of taxation.
-
Value Added Tax (2003)
Value added taxes are based on the economic activity or the value that businesses add to the production of goods and services. The tax base is final sales less the cost of goods sold or the cost of materials used as inputs. The SBT is a modified VAT.
- In Europe, where the VAT is levied by most national governments, it is seen as a consumption tax which is roughly equivalent to a national sales tax.
- In a subnational unit of government such as Michigan, however, the SBT is generally thought of as a tax on businesses—rather than on consumers. In reality, any business tax imposes some economic costs on both producers and consumers.
- Any business tax imposes some economic costs on both producers and consumers.
- The basic premise underlying value-added taxation is relatively straightforward: taxes should be treated as just another cost of doing business, and all business activity should be taxed at the same rate, regardless of whether a firm earns profits (see reference).
-
The tax applies equally to every business, and the amount of the tax was independent of the legal form of the business, the nature of the business and the particular production of financing means chosen by the business.
-
Net Income/Profits Based Tax
-
Michigan Tax History prior to 2003
- The first tax of a general nature to be levied on businesses was the Business Activities Tax (BAT)
in 1953,
in the face of a budget deficit. This deficit was in part a result of a 1946 constitutional amendment which had diverted two-thirds of sales tax revenue to school districts and local governments
. The BAT was an Income-type VAT
. The tax rate was initially set at 0.4 percent and had risen to 0.75 percent. The tax allowed for a $10,000 exemption, a gross receipts deduction, a labor intensity deduction, and a net income credit and did not allow for the immediate deduction of expenditures for capital investment. Financial institutions and insurance companies were exempt from the BAT because they were subject to various other taxes; public utilities faced a lower tax rate.
-
BAT was repealed
and the Corporate Income Tax adopted
in 1967. Both were proposed by Governor Romney
in an effort to avoid a budget deficit. He stated Business taxes hampered economic growth and discouraged new businesses, and are an unreasonable burden on operations with a small profit margin as opposed to income/profit taxes. Organized labor favored it, small and service businesses disliked it.
- In 1976 switched to the Single Business Tax (
SBT
)
as Michigan faced another fiscal crisis starting in 1975. It was favored by high-profit manufacturers, retailers, financial institutions, and utilities, mainly because their taxes would be reduced. Multinational businesses favored the VAT because its adoption solved . . . major problems that they were concerned about. The SBT
replaced the corporate income tax, corporate franchise tax, personal property tax on inventories, business intangibles tax, financial institutions tax, insurance company privilege fee, and savings and loan company privilege tax. The final version of the tax contained a large number of compromises which were necessary to ensure adoption of the tax.
-
In 1987, the method of taxing insurers was completely altered.
- In 1996, legislation was enacted that ended all revenue sharing payments made from SBT
collections and income tax collections—replacing this funding at a reduced level with a statutory earmarking of sales tax revenue effective with fiscal year 1997. Inventory replacement payments continued, but were made from sales tax revenue.
- Legislation in 1999 initiated a phase-out of the SBT
. Retroactive to January 1, 1999, the tax rate was to be lowered by 0.1 percent annually.
- The SBT
value added tax was, however, was reinstated in 2003
. Part of the rationale was:
- The revenue generated by the corporate income tax had fluctuated so dramatically with the business cycle.
- The CBT /VAT would promote capital investment and improve Michigan’s business climate.
- It was apparent that "Legislative debate over the SBT
[Single Business Tax] was influenced by competing groups of businesses who stood to either gain or lose under the new tax and a plethora of proposals to address these concerns
."
- The first tax of a general nature to be levied on businesses was the Business Activities Tax (BAT)
in 1953,
in the face of a budget deficit. This deficit was in part a result of a 1946 constitutional amendment which had diverted two-thirds of sales tax revenue to school districts and local governments
. The BAT was an Income-type VAT
. The tax rate was initially set at 0.4 percent and had risen to 0.75 percent. The tax allowed for a $10,000 exemption, a gross receipts deduction, a labor intensity deduction, and a net income credit and did not allow for the immediate deduction of expenditures for capital investment. Financial institutions and insurance companies were exempt from the BAT because they were subject to various other taxes; public utilities faced a lower tax rate.
-
Michigan Taxation after 2003
- In July 2007
, the Michigan Business Tax (
MBT
)
was signed into law by Governor Jennifer M. Granholm
. It imposed a 4.95% Business Income Tax
plus a Modified Gross Receipts Tax
at the rate of 0.8%
. Insurance companies and financial institutions paid alternate rates.
- In December 2007
, Public Act 145 amended the MBT
to totally replace the pr
ior
Single Business Tax (
SBT
), under Governor Jennifer M. Granholm.
-
In
2010
when Governor Snyder campaigned for Governor, falling tax receipts was a major issue. Snyder unveiled his Executive Order for reducing the fiscal year 2015 budget to balance the revenue shortfall that resulted from previous business tax credits
.
http://www.michigan.gov/ snyder /0,4668,7-277-61409_71099-347306--,00.html
- In January 2012, the Michigan Business Tax (
MBT
) was itself replaced by the Corporate Income Tax (CIT)
. Businesses could still elect to file under the prior MBT
. See the Michigan CIT fact sheet.
- "The widely despised MBT
— c
reated as a replacement for the similarly reviled Single Business Tax - died... It was four years old. The tax's demise was the product of a relentless political assault
by Gov. Rick Snyder
, who hammered the tax as a "job killer" in 2009.
http://www.annarbor.com/business-review/ so-the-michigan-business-tax-is-dead-will-it-create-jobs /
http://www.annarbor.com/business-review/rick-snyder-republicans-unveil-new-budget-proposal-reducing-pension-tax-proposal-maintaining-busines/
http://www.annarbor.com/business-review/ rick-snyder-calls-for-elimination-of-michigan-business-tax /
- "Michigan Business Tax Replaces SBT**
(167-03) 167-03 MichiganBusinessTaxreplaceSBT.pdf
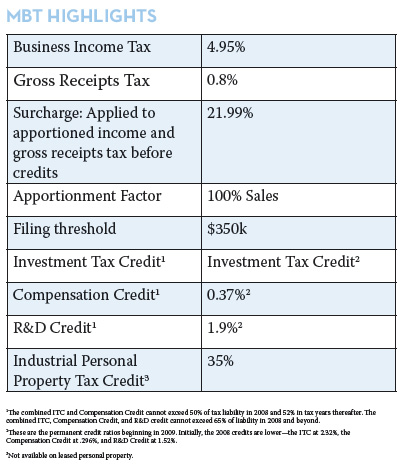
- "The widely despised MBT
— c
reated as a replacement for the similarly reviled Single Business Tax - died... It was four years old. The tax's demise was the product of a relentless political assault
by Gov. Rick Snyder
, who hammered the tax as a "job killer" in 2009.
- Snyder had supported Michigan's cuts to the teacher retirement
and municipal retiree health care
systems, reducing the state's liabilities.
To Pay for business tax cuts
, the Legislature approved Snyder's recommended phase-in of a pension tax
, a massive reduction in tax credits for the poor
, and other income tax code changes. Snyder sought to get the Legislature to approve big cuts in K-12 funding
, higher education funding
, municipal revenue sharing
and other sources.
- In July 2007
, the Michigan Business Tax (
MBT
)
was signed into law by Governor Jennifer M. Granholm
. It imposed a 4.95% Business Income Tax
plus a Modified Gross Receipts Tax
at the rate of 0.8%
. Insurance companies and financial institutions paid alternate rates.
-
This clearly has never been about the economic viability of a Gross Business Tax (without deductions) in Michigan. It is about the lack of political will to properly institute one without crippling compromises or inappropriate tax levels. "Tax changes allowed Pass-thru and Gas Taxes in MI that
shifted the burden of taxes from Corporations to Individuals
, and increased Corporate Administrative and Investor profits.". It would be an amazing argument for MacDonald's
Restaurants to say "we favor tax policy that increases MacDonald's
taxes and decreases Burger King's".
“Tax cuts... are only effective in recessions, when they raise employment by around 0.6% and income from employment by around 1% for every percentage point cut in the tax rate.” ( 119-04 )
- As an aside, an interesting rationale for excluding non-proft
organizations is offered: (123-01)
- "Nonprofit and governmental organizations, however, have never been subject to the tax. Nonprofit organizations have been exempted because they are thought to provide services which serve society as a whole, while governmental organizations have been exempted to avoid the circular process of government taxing itself."
-
However, in practice today, non-profits concentrate on society as a whole, but push tax-free money into narrow lobbying agendas which bring windfall sums back to the interest group.
- I commend (article 123-01) to our CA State Legislators
the excellent interesting exploration about the rationale for Business taxation in their adoption of its S
ingle Business Tax
(
SBT
, a Value Added Tax, and its history of the ping-pong taxation experiments in Michigan from 1946 to 2003 and beyond. Michigan has a storied history dealing with Health Care worth examining.
-
According to the Tax Foundation article, "In the past ten years, four states that had utilized Gross Receipts Tax eliminated them. As outlined here, this has been part of the ebb and flow largely determined by Legislature mistakes and shortfalls in their Budgets:
-
Further Comments on State Experiences with the Taxation
-
Arizona
- Arizona, which has a Transaction Privilege Tax
(Gross Receipt Tax) since 2011, was
ranked the #1 most competitive state in the mountain region
, and Area Development magazine has awarded Arizona a 2017 Gold Shovel Award as the top state in economic development in the five-million to eight-million population category.
- Arizona, which has a Transaction Privilege Tax
(Gross Receipt Tax) since 2011, was
ranked the #1 most competitive state in the mountain region
, and Area Development magazine has awarded Arizona a 2017 Gold Shovel Award as the top state in economic development in the five-million to eight-million population category.
-
New Hampshire
- New Hampshire does not have a personal income tax or a state sales tax but does impose a tax on interest and dividends, fiduciaries, certain business entities (5%), and a Meals and Rooms tax (9%). As such, the majority (over 20%) of state tax revenue is generated from the Business Profits Tax
(“
BPT
”)
and Business Enterprise Tax (“BET”),
which are assessed on business conducted in the State. New Hampshire adopted the value-added type tax (the Business Enterprise Tax) in 1993 at a rate of (0.25 percent), as a complement to its Business Profits Tax (
BPT
)
. (134-09)
- In general terms, New Hampshire’s Business Profits tax (
BPT
)
is a flat 8.5%
tax on
net federal taxable income
from business activity in the state, applied before any federal net operating loss or special deductions, and with various state-specific additions and deductions. Businesses with $50,000 or less in New Hampshire gross receipts are not required to file a BPT
return. (134-01)
v - The additional Business Enterprise Tax (BET)
is based on a business’s “enterprise value tax base.” This is defined by the Department of Revenue Administration as “the sum of all compensation paid or accrued, interest paid or accrued, and dividends paid by the business enterprise, before special adjustments and apportionment
.” The BET rate is 0.75%
. A business is required to file a BET return if its enterprise value tax base is more than $100,000; or it has more than $200,000 of gross business receipts.
- New Hampshire currently holds the 10th highest corporate income tax in the country
and supporters say the high rates make it difficult for New Hampshire to compete with neighboring states.
- I am struck by the similarity of arguments for States altering their tax structures so as to "compete with neighboring states." It sounds a lot like the mantra under Robert McNamara
at the Ford Motor Company, and now in Health care calling for "managed competition" between the Units.
- The greatest problem for any control system is corruption
; right of passage
, and succession
, and both complexity and secrecy enable corruption. Top-down versus bottom-up issues convergeon
where to place the decision points.
- I am struck by the similarity of arguments for States altering their tax structures so as to "compete with neighboring states." It sounds a lot like the mantra under Robert McNamara
at the Ford Motor Company, and now in Health care calling for "managed competition" between the Units.
- "The failure of General and Education Fund revenue to rebound
since the economic downturn in inflation adjusted terms can largely be attributed to declines within four discrete revenue sources: New Hampshire’s twin business taxes, the business profits tax (
BPT
) and business enterprise tax (BET); the statewide property tax; the interest and dividends tax; and the communications services tax... each of these sources has dropped substantially in inflation adjusted-terms since FY
2008... Proposed
reductions in the rates of the BPT
and BET would likely extend the preceding trend
into the next decade
."
(134-05)
- While some proponents of lower business tax rates assert that such changes will allow companies to retain more of their earnings and create greater incentives to invest and expand in New Hampshire, the weight of the empirical evidence suggests that across the- board rate reductions are not an effective way to stimulate economic growth
.
- One reason is that state and local taxes paid by corporations are a very small share of their total expenses. Moreover, businesses’ investment decisions are mostly driven by anticipated demand for their products
, not by small reductions in their marginal tax rates. Finally, surveys of business executives suggest that
what is most important to them in locating their businesses is the quality of the local labor force and physical infrastructure
, rather than corporate tax rates
.
v - Accordingly, claims that lowering business tax rates would spur faster growth in the underlying base of the BPT
or BET and thus help to counter the trend depicted here have little merit. "Businesses [also] prefer a more stable, clear and predictable tax policy and administration. A major impediment to business is a tax climate that changes and reacts to each budgetary or legislative session." (134-05)
- While some proponents of lower business tax rates assert that such changes will allow companies to retain more of their earnings and create greater incentives to invest and expand in New Hampshire, the weight of the empirical evidence suggests that across the- board rate reductions are not an effective way to stimulate economic growth
.
- New Hampshire does not have a personal income tax or a state sales tax but does impose a tax on interest and dividends, fiduciaries, certain business entities (5%), and a Meals and Rooms tax (9%). As such, the majority (over 20%) of state tax revenue is generated from the Business Profits Tax
(“
BPT
”)
and Business Enterprise Tax (“BET”),
which are assessed on business conducted in the State. New Hampshire adopted the value-added type tax (the Business Enterprise Tax) in 1993 at a rate of (0.25 percent), as a complement to its Business Profits Tax (
BPT
)
. (134-09)
-
Washington State
- Washington State levies the nation’s oldest broad-based Gross Receipts Tax. First enacted in 1933 and significantly revised in 1935, the state’s Business & Occupation (B&O) Tax
illustrates many of the flaws inherent in taxing gross receipts. In 2002, a tax reform commission appointed by the state’s legislature concluded that the B&O tax results in substantial tax pyramiding and is highly non-neutral across products and industries, violating basic principles of good tax design. From the committee’s report: “
Neutrality requires that a tax system minimize the opportunities and incentives for taxpayers to alter their decisions in order to take advantage of differential tax treatment of economic activity (This is termed a Moral Hazard
).
“The finding for the Washington State tax system is that it causes substantial nonneutralities for both businesses and household s. The pyramiding of the B&O tax creates the main non-neutralities for businesses. Pyramiding of taxes is the payment of taxes by different companies on the same goods or services. This occurs when goods or services of one company are inputs for another’s production and/or sales. Thus, a tax is paid multiple times on a product as it moves through the production chain.
A way around this would seem to be balancing the Gross Receipts Tax with a Business Income Tax at each step.
- “The B&O tax pyramids an average of 2.5 times, but this rate varies considerably across industries. The B&O tax on many services pyramids at about 1.5 times, whereas for some types of manufacturers the rate of pyramiding is over five or six times. This causes effective B&O tax rates (the rate paid on the value added to goods and services by an enterprise) to vary considerably from industry to industry.” The commission found the B&O tax causes tax pyramiding of up to 6.7 times on some manufacturing industries, while some services are taxed just 1.4 times. Effective tax rates vary from less than 1 percent on retail trade to more than 3 percent on electric and gas utilities, leading to potentially large economic distortions in the state’s economy
.
-
The following table
illustrates the sharp degree of tax pyramiding under the B&O tax, and the wide variation in effective tax rates on industries.
- “The B&O tax pyramids an average of 2.5 times, but this rate varies considerably across industries. The B&O tax on many services pyramids at about 1.5 times, whereas for some types of manufacturers the rate of pyramiding is over five or six times. This causes effective B&O tax rates (the rate paid on the value added to goods and services by an enterprise) to vary considerably from industry to industry.” The commission found the B&O tax causes tax pyramiding of up to 6.7 times on some manufacturing industries, while some services are taxed just 1.4 times. Effective tax rates vary from less than 1 percent on retail trade to more than 3 percent on electric and gas utilities, leading to potentially large economic distortions in the state’s economy
.
- Note, however, that the two highest tax pyramiding sectors above are exempted from taxation in SB-562/2.3.
- Washington State levies the nation’s oldest broad-based Gross Receipts Tax. First enacted in 1933 and significantly revised in 1935, the state’s Business & Occupation (B&O) Tax
illustrates many of the flaws inherent in taxing gross receipts. In 2002, a tax reform commission appointed by the state’s legislature concluded that the B&O tax results in substantial tax pyramiding and is highly non-neutral across products and industries, violating basic principles of good tax design. From the committee’s report: “
Neutrality requires that a tax system minimize the opportunities and incentives for taxpayers to alter their decisions in order to take advantage of differential tax treatment of economic activity (This is termed a Moral Hazard
).
-
Maryland
We are not able in the present work to appropriately review the Health System in Maryland, which continues to undergo change. Maryland is further on the path towards Single payer, having established its All-Payer Program. There is increased activity in the State about a Single=Payer System. It would be worthwhile to scrutinize their efforts for lessons learned. Comments included here are a sampling.
-
Single-Payer? : Healthcare-Now of Maryland
( 149-02 ) 149-02 Single-Payer - Healthcare Now of Maryland.pdf <<<OPEN
-
Can we afford such a [Single Payer] System?
In the long run, we will not be able to afford any other kind of system. Single-payer saves money by
decreasing administrative costs, eliminating unnecessary expenses like large CEO salaries,
advertising, profits, dividends, etc. and enabling negotiations for pharmaceuticals, medical equipment
and hospital rates.
-
How would Single-Payer work?
A public agency would be created to organize health care financing, collecting money and paying the
bills. Government is very good at these two tasks. The health care insurance industry would be
eliminated as we currently know it. Insurance companies currently intrude as a barrier between
patients and the doctor, destroying the therapeutic relationship. Health care costs would further be
controlled by negotiation with drug companies, hospitals, doctors and other providers creating a
system that would be reasonable and fair to all.
-
How much does this overhead add up to?
At least 31% of healthcare expenses in the United States go for administrative expenses, which
means that less than 70 cents of every dollar spent for health insurance is available for actual health
care. With a Single-Payer system over half of administrative costs could actually be used for health
care. The savings amount to about $400 billion per year nationally,which is way more than enough to
provide comprehensive health care for the 48 million uninsured and the 10’s of millions who are
underinsured.
-
Can we afford such a system?
In the long run, we will not be able to afford any other kind of system. Single-payer saves money by
decreasing administrative costs, eliminating unnecessary expenses like large CEO salaries,
advertising, profits, dividends, etc. and enabling negotiations for pharmaceuticals, medical equipment
and hospital rates.
-
Would my doctor or hospital be assigned to me?
No. You would be free to choose any doctor or hospital or other service that you need.
-
Wouldn’t this be socialized medicine?
No. The government would not own the health care system. Just as the government does not own the
health care system with Medicare. Doctors, hospitals, drug companies, etc. would all remain private
and be owned as they are now. However, they would have to negotiate with the public agency for
what they could charge for their products and services and if they choose to remain outside of the
system they would be free to do so.
-
Can we afford such a [Single Payer] System?
- Maryland’s Single Payer Push May Save Medicare Billions - (Kate Rogers, FoxBusiness
2014)
(149-03) 149-03 Maryland’s Single Payer Push May Save Medicare Billions | Fox Business.pdf <<<OPEN
"Maryland is the only state in the nation that has set its own rates for hospital services, which it has done for the past 36 years . All patients also pay the same rate for services at hospitals throughout the state under its current Medicare waiver. The initiative
allows Maryland to set global budgets, and alternative approaches to payment, according to a release from the governor’s office."
-
Has Maryland found a solution to the U.S. healthcare cost crisis? (Becker)
( 149-05 ) 149-05 Has Maryland found a solution to the U.S. healthcare cost crisis?. pdf <<<OPEN
- Dr. Mortensen [assistant professor in the University of Maryland's Department of Health Services Administration in College Park] confirms that physicians "feel sort of left out," since gainsharing hasn't been established for them at a lot of hospitals: "Physicians don't really feel that they have all the support that's necessary. The state's going to have to keep in very close contact with physicians and pay attention to their concerns."
- As for why the all-payer system in Maryland hasn't met with a similar fate, Dr. Sharfstein offers a couple of reasons: "There has been a degree of collaboration between the hospitals and the state and the payers that has really been remarkable over the last several decades. There's a real feeling that everybody's in this together. And then I think the other major factor is there's a provision in the Social Security Act that assures Medicare participation under certain conditions. It's a combination of some provisions in law that are really helpful and the spirit in the state."
- Therefore, Maryland and CMS agreed on a new initiative to update the 36-year-old Medicare waiver. Under the new system, the all-payer system is based on containing per capita total hospital cost growth rather than payment per admission. The state has agreed to limit its annual all-payer per capita total hospital cost growth to the 10-year average growth rate of the state's economy, 3.58 percent, according to CMS . Additionally, Maryland will transition essentially all of its hospital revenue into global payment models during the five-year initiative.
- Although it's still not a perfect system, "in terms of being a fundamental turning upside down of the payment incentives…it's a very positive thing," says John Deane , president of Advisory Board Consulting at The Advisory Board Company. "We're noticing institutions in Maryland are having an awakening of having the imperatives to deliver value both in terms of cost and quality. They're excited that the new payment methodology will reward that."
-
"I've been in this business since 1978, and this is probably the most meaningful thing I've ever seen in controlling costs without it affecting quality," Mr. Mullen [president and CEO of Mercy Health Services] says. "We don't have it solved, but I think we're moving in the right direction."
-
Financing the Maryland Health Security Act (2013)
Gerald Friedman Professor of Economics The University of Massachusetts at Amherst
( 149-11 ) http://www.md.pnhp.org/docs/ Maryland-single-payer-study.pdf
A comprehensive discussion about financing the Maryland HEalth Security Acto of 2011
-
Maryland Gross Receipts Tax Overview (2009)
Presented to the Maryland Business Tax Reform Commission
Andrew Schaufele Bureau of Revenue Estimates
( 149-13 ) 149-13 Gross Receipts Tax Overview - 9_10_2009_Gross_Receipts_Tax_ Presentation.pdf- tax on the privilege of doing business within the state or as a tax on business activity.
-
Presents many Pros and Cons.
-
Maryland All-Payer Model (1/2018)
( 149-30 ) 149-30 Maryland All-Payer Model | Center for Medicare & Medicaid Innovation.pdf
-
HSCRC
Update on Maryland's Health Care Transformation (3/2017)
( 149-34 ) 149-34 HSCRC PowerPoint Presentation - 2017-03-09 Pres - HSCRC Update final.pdf
149-34a MD to date 2018. pdf
-
Single-Payer? : Healthcare-Now of Maryland
-
Arizona
back
back
- Current Medicare cost comparison, supplemental insutance
creates complexity! This summary article from the Medicare website outlines how the costs and benefits are partitioned for the patient:
- Medicare Parts A, Part B, Part C, Part D
140-09 Medicare 2017 costs at a glance _ Medicare . pdf <<< OPEN
- Medicare Parts A, Part B, Part C, Part D
- STANDARD MEDICARE (SM)
- FEE-FOR-SERVICE (FFS)
- Medicare PART A (Hospital)
- Medicare PART B (Non-Hospital/Services) ( FFS - 70% of Medicare Recipients)
- Access to any provider - No restrictions in-network or in-panel.
- Typically covers 80% of treatment cost ( 20% Co-Pay cost to patient without Advantage supplemental)
- Supplemental Insurances (
MediGap
, Medicaid, or Retiree Secondary Insurance) fills in virtually all remaining costs, so enrollees essentially see no out-of-pocket..
- MEDICARE ADVANTAGE (MA)
- MANAGED CARE (HMO and PPO - 30% of Medicare Recipients)
- Medicare PART
(Alternative Plans includes A and B
and allows D
)
- PPO
ADVANTAGE
[PREFERRED PROVIDER ORGANIZATION]
Advantage PPO covers a smaller in-network and sometimes out-of-network, by paying higher up-front premiums than HMO unless they choose higher out-of pocket. The Networks offered often appear more extensive than they actually are. Up-front deductibles and co-pay requirements for each individual service rendered are intended to ensure some cost sensitivity. This also restricts access and increases administrative costs . - HMO ADVANTAGE
[HEALTH MAINTENANCE ORGANIZATION]
Advantage HMO covers in-network only, paying lower premiums than PPO and FFS . Patients go only to in-panel providers.
- PPO
ADVANTAGE
[PREFERRED PROVIDER ORGANIZATION]
- In Medicare Advantage
, the federal government hires private insurance companies; they in turn contract with service providers, using money collected from Medicare enrollees thru a payroll tax. This extra layer of insurance administration diminishes the doctor-patient relationship and strengthens outside influences, because so much in Health Care is determined by control and flow of money. It saves money only by reducing services.
- Advantage HMO and PPO
initial premiums are less, but out of pocket can be much more
, as high as $6,000. Out of network is not covered for HMO. Some face unexpected thousands of dollars in uncovered costs having been switched into an Advantage plan, and usually have to go through medical underwriting for re-enrollment in a MediGap
plan. A serious health condition can prevent them from getting approved.
- Part C Advantage is required for enrollee to participate in Part D enrollment.
- Advantage plans can restrict access to Docs who give more complete ("costly") care. Patients have more kimited
ability for patients to assess the quality of care because there is nothing to compare to. Access to specialists is gated, which is not appreciated until need to access services. Plans re-file their benefit lists with Medicare every year, so coverage benefits are constantly changing, requiring a lot of accouting
.
- Advantage case managers can dictate treatments and denial of service. Some plans review every claims, requiring duplicative paperwork. Increasingly the best providers are refusing to take Advantage.
- Advantage pays Providers less than Standard Medicare
(This is not well known to participants. They see the lower premiums, not the limited care options).
- Taxpayers subsidize Medicare Advantage, increasing the Taxpayer Burden. Patients don't see the actual costs of the increased benefits because it is subsidized.
- Advantage Plans have high Marketing costs, charging more for overhead and access, thus generating greater
profit. Advantage is difficult to audit; CMS reviews less than 1 percent of all networks.
- MEDICARE PHARMACY SUPPLEMENTAL - Medicare Part D
(Drugs)
- Individual Drug costs are Highly subsidized by Taxpayers
- Contribute a large fraction to cost increases
- Has been a windfall to the Pharmaceutical Organizations
- MEDICARE COSTS AND ISSUES
- History of Managed Care in the United States
- Congress passed the HMO Act in 1973 under President Nixon. In 1969, Kaiser was the only major HMO in the Country. Combined with Medicare, the HMO Act eventually eliminated the market for affordable Individual Health Insurance. Managed Care plans mushroomed under federal and tax-payer subsidies
. By 1999 HMOs accounted for 40% of plans. With the collapse of the Hospital Systems and Government bailout this decreased to 27% by 2009, but was back up to 35% by 2015.
- Medical Savings Accounts (
MSA
/
HSA
) were later introduced. Rather than making Individual Health Insurance profits 100% Tax Deductible, it funds a portion as tax Insurance and a portion as a Savings Account, both with pretax dollars. It isolates an individual from some of the Hi-Risk Group Financial Costs, but also some of the Large Group Financial subsidy (high deductibles).
- Health Insurance at present
co-mingles
Business, Employer, Employee, Retirement Funding, Banking, Finance, Tax and Government components in ways that are not at all transparent or quantifiable. Individual choice is controlled by Government Law and the Tax code, which may be why some are opposed to Universal Care. It is impossible to control cost inputs with Managed Care because Costs are correlated and constantly changing. It is impossible to measure the care outputs because they are complex and correlated.
- Medical Liability standards increase insurance costs, but as demonstrated with other insurances is absolutely required.
- Congress passed the HMO Act in 1973 under President Nixon. In 1969, Kaiser was the only major HMO in the Country. Combined with Medicare, the HMO Act eventually eliminated the market for affordable Individual Health Insurance. Managed Care plans mushroomed under federal and tax-payer subsidies
. By 1999 HMOs accounted for 40% of plans. With the collapse of the Hospital Systems and Government bailout this decreased to 27% by 2009, but was back up to 35% by 2015.
- MedicaRe
is FedeRal
InsuRance
for Retirees
, paid by workers out a Payroll (Medicare) Tax with Social Security. A significant part of Medicare coverage is provided out of Tax Revenues as well.
- MedicAid
is StAte
AssistAnce
for Low Income
Residents
(with variable but minimum 50% Federal matching).
- Health Care Cost has multiple component
s that are not easily separated from each other. for instance:
[Care]+[ CareOverhead ]+[ CareProfit ] and [Admin]+[Admin Overhead]+[ AdminProfit ]+[Financing].
- Many private insurers piggyback on Medicare’s provider payment system
. In 2006 some 75 percent
of (non-Medicare) private insurance plans u
sed the Medicare physician fee schedule as the basis for payments to Physicians (Part B)
. Similarly, the vast majority of private insurers use Medicare’s Diagnostic-Related Group (
DRG
) payment structure to make payments to hospitals for inpatient services (Part A).
- FFS
(Fee-For-Service) has low administrative overhead
. HMO has high administrative overhead
. PPO
has something in between
, with the most complexity and opportunity to shift costs and profits. It also maintains some patient choice.
- Open-ended tax subsidies
of employer-sponsored insurance encourages increased cost. The gap in Tax benefit gives large employers more leverage over workers.
- Employed health premiums were made 100% Tax Deductable in 1942 (during WWII).
- Self-employed
insurance is 50% Tax Deductible
, and non-employed have no deduction as well as no access to Group discounts.
- Unrestricted Health Care for Seniors led to an "unprecedented frenzy of spending", although much was from an improvement in needed care. The Amy Finkelstein
Study (2006) indicated that Medicare, and federally subsidized third-party insurance caused about a 300%
real increase in per capita health care costs in the United States in the 2 decades after Medicare enactment in 1965. Although Physician Cost increased some
35%
over this period, Administrative cost went up comparably
1000%
.
- Additional non-retiree health expenditures associated with the elderly and disabled on Medicare approached 40 percent in 2004. These require additional expenditures from State and Federal Taxes collections separate from Medicare.
- Medicaid pays for nearly half of all US births (2013). (152-01)
- History of Managed Care in the United States
- MEDICARE COMMENTARY
- The Capretta
Paper (2013) argues that effective cost control requires Delivery-System reform.
( 14-06 ) 14-06 The Role of Medicare Fee-for-Service in Inefficient Health Care Delivery - Ethics & Public Policy Center print.pdf
- Insurance-Driven Systems fail to control Delivery-Systems
, because they make decisions before there are facts for each patient are determined. Bypassing Physician-Decision-Systems has been a costly mistake (even with the Obama
Patient Protection and Accountability Care Plan / PPACA
approach). The use of capitation
, bundled payments
, and pay-for-performance
all ration care and worsen outcomes utilizing the Managed Care approach which uses only a subset of the available information relevant to that patient.
- Capretta
argues that "Medicare FFS
remains essentially a claims-paying enterprise that does not discriminate among appropriately licensed providers of services." and "does not pick winners and losers." That may be true, but patients themselves show tremendous discrimination over time when they are given actual choice among all providers, rather than pick from a closed panel that is mass marketed.
- Although touted to decrease costs, the average Medicare Advantage plan provides Medicare benefits at 98 percent of fee-for-service costs. It reimburses less to Physicians, however, and many refuse to contract with Advantage Plans.
- The flawed assumption is that 'low quality' providers are 'high cost'. Lower quality providers get more patients because the insurance company locks out competition. If licensed providers are adequately trained, why should choice cost more? Are the better providers charging too much? Physicians who spend decades of their time Academically and Clinically learning and yes, practicing Medicine, should not just be tossed to the junk pile. We don't start out perfect, we become better.
- High-quality contradicts Low-cost. Does a Rolls Royce cost less than a Yugo
, even in efficient mass production? Better care costs more, but Insurance administration should not. Does it cost more to list a good doctor over a bad one? Does having 500 Medicare Advantage Insurance Plans provide any economy of scale, rather than increased overhead?
- Should Health Care be a civil service Pay-for-Administration Jobs program? Why not add Pay-For-Training (which does not now appear in fee schedules) with the Pay-For-Service program? Farm subsidies to produce less may be an approach in milk farming, but paying more to do less Medicine is an absurdity. Why do we expect non-physicans
can competently evaluate physicians, when there are so many variables? Even Physician teachers require extensive training and experience to do that.
- In conclusion Capretta
states, "The federal government’s health care administrators have been trying for many years to bring change to Medicare through a regulatory framework. The available evidence indicates that this approach has not worked because the fundamental political dynamic pushes toward a fragmented delivery system that is built on volume, not quality. New efforts to change Medicare’s basic dynamics may prove to be modestly more effective than previous efforts, but
there is no real prospect that these efforts will fully solve the problem
. In the end, real change will almost certainly require a more fundamental reform..."
- It is not the fragmented delivery system that fails, it is the Administrative overuse, secrecy and lack of audit that does so. We can't learn to improve our mistakes when our corporations force us to hide them.
- A Private Office is actually shown to be more cost effective than managed care, especially when utilizing NP's. Why do studies neglect this option when making comparisons?
- All this
supports enacting a California State Level Single Payer.
- The Capretta
Paper (2013) argues that effective cost control requires Delivery-System reform.
back
back
- Credibility problems and dearth of comprehensive Taxation and Earnings Data
- A problem in producing this HSC
Workbook is that although there is prolific information expounding opinions, it requires extreme and skilled effort get actual Data on Health Care and its financing. When doing online searches much of the state data appears in articles from criticized organizations such as the the Tax Foundation, which requires extreme scrutiny.
- Corporate Businesses are in some analogy structured as mining operations, whether as for gold, or for other tangible assets, only needing to address the parts of the issue that affect their own profit. They do not have to create actual value, but concentrate on funneling money to their cause, or additionally destroy those who could reduce the value of the asses they accumulate. This needs to change in Medicine.
- A problem in producing this HSC
Workbook is that although there is prolific information expounding opinions, it requires extreme and skilled effort get actual Data on Health Care and its financing. When doing online searches much of the state data appears in articles from criticized organizations such as the the Tax Foundation, which requires extreme scrutiny.
- California Association of Health Underwriter
s
(For-profit Insurance Community, Right-of-Center)
( 110-02 ) 110-02 California’s Single-Payer Health Care Plan Would Cost More Than the State’s Whole Budget - Hit & Run _ Reason.pdf
- Association is listed as one of the organizations opposing SB-562 , so is not a neutral source. Issued a press release opposing SB-562
- Association favors continuing the Private Health Insurance System, as is.
- States "Three out of Four of California Voters are Opposed to a Universal Single Payer Health Care System". ( contradicted )
- States "SB-562 is a cost burden to families". ( contradicted )
- States SB-562 requires $179 billion in new taxes. ( contradicted )
- States SB-562 lowers the quality of care. ( already problematic )
- States SB-562 restricts funding Research funding. ( already problematic )
- States voters are less likely to support SB-562 knowing the cost to Californians in new taxes. ( disingenuous - the costs are the same with increased coverage, just will come from sales tax base, rather than employer payroll tax with its overhead and difficulties )
- States SB-562 is a government run Health System (
false
)
- SB-562 funding is administered by a board appointed by the state government . Neither Government, nor the Board run the hospitals or offices giving care. In fact, with a plan of fee-for-service the government has less to say about the system than under a socialized delivery system, since all parties have access to the pricing structure and can negotiate or sue for inadequate reimbursements.
- We find choice of physician is sometimes a concern of voters on Medicare, who are covered separately from SB-562 so is not a realistic argument. Physician access is already an issue.
- Rebuttal from
the SB-562 Senate Floor Analysis:
23-W 7.05.27 Senate Floor Analyses.pdf- "
California has a chance to lead the rest of the nation toward a health care model that is less expensive and provides better coverage."
- "
California has a chance to lead the rest of the nation toward a health care model that is less expensive and provides better coverage."
- Franklin Center for Government and Public Integrit
y (Non-profit, Right-of-Center)
- Online nonprofit news organization in the United States that "publishes news and commentary from a free market, limited government perspective"
on state and local politics. The Franklin Center publishes Watchdog.org
, a network of state-oriented websites
. The Franklin Center is an associate member of the State Policy Network, a consortium of conservative and libertarian think tanks which focus on state level policy
- Online nonprofit news organization in the United States that "publishes news and commentary from a free market, limited government perspective"
on state and local politics. The Franklin Center publishes Watchdog.org
, a network of state-oriented websites
. The Franklin Center is an associate member of the State Policy Network, a consortium of conservative and libertarian think tanks which focus on state level policy
- Eric Boehm
(
Blogger
- Right of Center)
- Reporter for Reason contributer
. "Received a bachelor’s degree from Fairfield University in 2009. He has also lived in St. Paul, Minnesota; Rochester, New York; and Brussels, Belgium. When he steps away from the computer, he enjoys drinking craft beer and good gin, cheering for an eclectic mix of favorite sports teams (mostly based in Philadelphia), updating his list of TV shows he intended to watch but never did, reading and traveling to new places."
- Major criticism of SB_563 (Don’t Fund California Single-Payer Health Care With a Gross Receipts Tax - Hit & Run May and June 2017)
( 110-02 ) 110-02 California’s Single-Payer Health Care Plan Would Cost More Than the State’s Whole Budget - Hit & Run _ Reason.pdf
( 110-03 ) 110-03 Don’t Fund California Single-Payer Health Care With a Gross Receipts Tax - Hit & Run _ Reason HL.pdf
- Ambiguous questions cited in the surveys include:
- require many Americans to pay more taxes ( saves costs )
- give the government too much control over health care ( private providers )
- eliminate or replace the current health care law (what does that have to do with it?)
- Ambiguous questions cited in the surveys include:
- Reporter for Reason contributer
. "Received a bachelor’s degree from Fairfield University in 2009. He has also lived in St. Paul, Minnesota; Rochester, New York; and Brussels, Belgium. When he steps away from the computer, he enjoys drinking craft beer and good gin, cheering for an eclectic mix of favorite sports teams (mostly based in Philadelphia), updating his list of TV shows he intended to watch but never did, reading and traveling to new places."
- Tax Foundation
(Nicole Kaeding
, Charles and David Koch, Oil Industry, Libertarian)
- The Tax Foundation was organized on December 5, 1937 in New York City by Alfred P. Sloan, Jr., Chairman of the General Motors Corporation
; Donaldson
Brown, GM Financial Vice President; William S. Farish
, President of Standard Oil Company
of New Jersey (Exxon); and Lewis H. Brown, President of Johns-Manville
Corporation, who later became the first Chairman of the Board of The Tax Foundation. The stated goal of the organization was "to monitor the tax and spending policies of government agencies".
( 119-02 ) about Us - Tax Foundation
- Note the above formal picture of the Tax Foundation members indicates a severe under-representation The United States diverse majority ethnicity.
- Note the above formal picture of the Tax Foundation members indicates a severe under-representation The United States diverse majority ethnicity.
- Beginning in 1990, the Tax Foundation "operate[d] as a separate unit" of Citizens for a Sound Economy
.
- Tax Foundation public position on Gross Business Tax by the States (see dispute of these claims ahead)
- (
117-04
) 117-04 Gross tax receipts TaxFoundation
_FF523_0 HL.pdf
- Four states—Indiana, New Jersey, Kentucky, and Michigan—each enacted gross receipts taxes, but repealed them after experiencing negative effects. New Jersey’s and Kentucky’s taxes lasted only several years. (However, see discussion providing evidence disputing these points).
- Enactment quickly results in economic problems, including reduced levels of transparency, competitiveness, neutrality, and fairness.
- Despite broad agreement that gross receipts taxes lead to many economic problems, some states have newly begun to consider them as a policy option.
- States exploring tax reform should follow the example of other states and exclude the gross receipts tax from their revenue toolkit.
- Tax Foundation Eventually split into Citizens for a Sound Economy, FreedomWorks
, Americans for Prosperity, (& Tea party movement)
- Citizens for a Sound Economy
- Established in 1984 by Charles and David Koch of Koch Industries. Ron Paul was appointed as the
first chairman of the organization. - Ron Paul was appointed as the first chairman of the organization.
- The CSE described itself as "hundreds of thousands of grassroots citizens dedicated to (1) free markets and limited government, and (2) the highest level of personal involvement in public policy activism."
- In 2002, the CSE designed its tea party movement website, though the movement did not take off until 2009.
- In 2003, Dick Armey became the chairman of CSE after retiring from Congress.[
- Previous position on Climate: "Acid rain is a "so-called threat [that] is largely nonexistent".
- In 2004, Citizens for a Sound Economy
split into two new organizations
, with Citizens for a Sound Economy being renamed
as
FreedomWorks
, and Citizens for a Sound Economy Foundation becoming
Americans for Prosperit
y
. Both organizations played key roles in the Tea party movement beginning in 2009.
- Established in 1984 by Charles and David Koch of Koch Industries. Ron Paul was appointed as the
- Citizens for a Sound Economy
- Economist Paul Krugman
has
characterized the Tax Foundation as "not a reliable source"
in criticizing the conclusions of a report it produced comparing corporate tax rates in the United States to those in other countries.
( 120-01 ) 120-01 Economist's View_ _The Greek Menace_. pdf
-
- Nicole Kaeding
of the Tax Foundation holds a Masters Degree in Economics, and writes for prolifically for organizations underwritten by the Oil and Gas Energy Companies (Koch Industries). The references in her papers self-refer, and limited to those who hold her similar views. It is stunning how limited the range of the resources appear. Her training is in finance as an undergraduate, and economics in a masters program. Much of the analysis required for finance requires advanced mathematics and statistics, and so creates the problem of relying on politically cued evaluations, rather than scientific or fundamentally sound ones. Selection bias is extremely difficult to identify.
- Reports commonly are extrapolated from older data, so is difficult to access and reach conclusions beyond the data.
- The Tax Foundation fails to communicate that corporate taxes actually paid have decreased
(they use maximum tax rates before allowed deductions) so that the rates quoted overestimate corporate tax liability.
- A “statutory” tax rate graph cited uses the maximum rate a corporation can pay in principle. But because corporate tax rules allow all kinds of deductions and exclusions, the statutory rate is a poor guide to the actual disincentives the corporate tax creates.
- Reports are limited in their failure to include robust sources, uses postings by individual bloggers
whose funding is from narrow Economic interests and limited scrutiny prior to publication.
- There is little to distinguish writings from Marketing products and even frank propaganda which is highly effective for the gullible American Population living within information bubbles.
- As well, Tax Foundation has stated that Michigan repealed its Gross Receipts Tax. Michigan has not had a Gross Receipts Tax
. Michigan has had a Value Added Taxes (
SBT
)
which is caculated
off of the Total Gross Receipts, so there has not been a Gross Receipts Tax with a pyramiding structure.
- The motto of the Tax Foundation is "Help us achieve our vision of a world where the tax code doesn't stand in the way of success." SB-562 supports this goal, as Health Coverage is removed from Employment, Worker Income Taxation and Tax subsidies on policies. It provides a broadly based, stable tax stucture
that, with the State Sales tax can provide a stable Health System as well.
- Nicole Kaeding
of the Tax Foundation holds a Masters Degree in Economics, and writes for prolifically for organizations underwritten by the Oil and Gas Energy Companies (Koch Industries). The references in her papers self-refer, and limited to those who hold her similar views. It is stunning how limited the range of the resources appear. Her training is in finance as an undergraduate, and economics in a masters program. Much of the analysis required for finance requires advanced mathematics and statistics, and so creates the problem of relying on politically cued evaluations, rather than scientific or fundamentally sound ones. Selection bias is extremely difficult to identify.
- Krugman
describes that the Foundation as using unweighted averages, which overweights small countries.
- Krugman
has accused the Tax Foundation of "deliberate fraud" in connection with a report it issued concerning the American Jobs Act. The Tax Foundation has published various responses to Krugman's
criticisms.
- In reviewing the available online literature, Paul Krugman's
arguments appear credible.
- "As a result, the US is actually a corporate tax haven, with the lowest
effective corporate tax rates of almost all the countries that participate
in the OECD . That's a little fact that the Tax Foundation apparently
doesn't want the American public to understand, since all its hype is in
terms of statutory rates and not in terms of effective tax rates.
- "The Tax Foundation does something else it often tends to do in setting
out its propaganda: quote one source as a definitive authority, without
mentioning conflicting conclusions from other respectable sources "
- "
TheTax
Foundation wants employees to believe that they are the ones who
"really" pay corporate taxes come. But we don't know the incidence of
the corporate tax, and there are a number of conflicting studies. Even
the studies that exist make a number of assumptions that may bring
their conclusions into doubt..... What we do know is that many
corporations have been making very high profits and paying low taxes,
and that the corporate contribution to the fisc is considerably less as a
percentage of GDP than it used to be, at the same time that wealthy US
taxpayers are paying astoundingly low overall effective tax rates on their
income, including very low rates on their income from capital, while they
are garnering an ever larger share of the income pie."
back
- "As a result, the US is actually a corporate tax haven, with the lowest
-
- The Tax Foundation was organized on December 5, 1937 in New York City by Alfred P. Sloan, Jr., Chairman of the General Motors Corporation
; Donaldson
Brown, GM Financial Vice President; William S. Farish
, President of Standard Oil Company
of New Jersey (Exxon); and Lewis H. Brown, President of Johns-Manville
Corporation, who later became the first Chairman of the Board of The Tax Foundation. The stated goal of the organization was "to monitor the tax and spending policies of government agencies".
back
-
They say, "Funding is not determined and is too expensive."
( 23-G ) 23-G 17.05.22 appropriations mccarthy.pdf <<<OPEN
( 15-0 ) 15-0 Pollin-Economic-Analysis-SB -562 HLa.pdf <<<OPEN
- Some have argued that the funding mechanisms are not included in the Senate passed Bill SB-562 on June 1, 2017.
- The Senate Appropropriations
Committee issued their comments on April 27th, 2017, which did not include their May 25th Funding Resticiion
Amendment, and the Extensive Pollin
Analysis issued in May 2017 just days before the SB-562 passed the Senate and moved to the Assembly.
- They say, "Single Payor
can't work and is Politically unfeasible."
- We are ignoring the history of Health Care Funding in the other States. In particular, Maryland has an "All-Payer" Fee-for-Service Program. Hospitals and Physicians appear quite pleased with this approach. Also, the legislation in place requires that if Single Payer can be shown cost-effective, it will automatically
replace the All-Payer System.
- We are ignoring the history of Health Care Funding in the other States. In particular, Maryland has an "All-Payer" Fee-for-Service Program. Hospitals and Physicians appear quite pleased with this approach. Also, the legislation in place requires that if Single Payer can be shown cost-effective, it will automatically
replace the All-Payer System.
-
They say, "
HHS
will never approve the necessary waivers."
- SB-562 "authorizes, under Section 1332 of the ACA
, waivers for state innovation under which states can seek federal approval to waive major provisions of the ACA
, including the requirement for Exchanges, QHPs
, premium tax credits and cost-sharing reductions, the individual mandate and the employer responsibility requirement, provided federal requirements for comprehensive benefits, affordability, and comparable coverage are met and the state proposal does not increase the federal deficit.
( 23-E ) 23-E 17.05.14Senate HealthHL.pdf <<< OPEN
-
"Medicare is funded by payroll taxes, premiums paid by individuals who enroll in various “parts” of Medicare (Part A is hospital services, Part B is medical services, Part C is Medicare Advantage plans, and Part D is prescription drug coverage) and general revenue. Authorizes the federal Secretary of the Department of Health and Human Services, to develop and engage in experiments and demonstration projects for specified purposes, either directly or through grants to public or private agencies, institutions, and organizations or contracts with public or private agencies, institutions, and organizations."
( 23-E ) 23-E 17.05.14Senate HealthHL.pdf <<< OPEN
- SB-562 "authorizes, under Section 1332 of the ACA
, waivers for state innovation under which states can seek federal approval to waive major provisions of the ACA
, including the requirement for Exchanges, QHPs
, premium tax credits and cost-sharing reductions, the individual mandate and the employer responsibility requirement, provided federal requirements for comprehensive benefits, affordability, and comparable coverage are met and the state proposal does not increase the federal deficit.
-
They say, "Employee Retirement Income Security Act of 1974 (
ERISA
)"
restricts State Actions
-
ERISA
is the 900-pound-gorilla standing in the way of state-based reform. It prohibits states from regulating most elements related to self-funded employer-sponsored health plans. According to the Kaiser Family Foundation, 61 percent of covered workers are enrolled in such plans. (These plans are heavily tax-payer subsidized. Companies pay for these benefits tax-free among advantage of ofering
such programs not available to private insured.
For Single-payer in Vermont, roughly $500 million worth of federal income taxes would be forgone, owing to the current tax treatment of employer-sponsored health insurance,” one report argued. A question is whether companies should profit from tax-exempt activity
).
- Kaiser, for instance, could still maintain its Care functions under SB-562, but it is true it would not be able to fund its Employer-based Insurance Business (HMO). Facilites
and Doctors would have to bill the State Trust Fund directly for Care given.
- The recent Supreme Court case, Gobeille
v. Liberty Mutual Insurance Co., shows just how much ERISA
can restrict states’ ability to act. The court found Vermont cannot require self-funded insurers to disclose basic data about claims for their all-payer database. To what degree the vague law would prevent different state reforms is a significant matter of debate that makes any planning difficult. State-based health care reform would be fairly easy if the state could simply require every employer to buy their employees the state-based, Medicare-like insurance policy or pay a large tax.
-
ERISA
is the 900-pound-gorilla standing in the way of state-based reform. It prohibits states from regulating most elements related to self-funded employer-sponsored health plans. According to the Kaiser Family Foundation, 61 percent of covered workers are enrolled in such plans. (These plans are heavily tax-payer subsidized. Companies pay for these benefits tax-free among advantage of ofering
such programs not available to private insured.
For Single-payer in Vermont, roughly $500 million worth of federal income taxes would be forgone, owing to the current tax treatment of employer-sponsored health insurance,” one report argued. A question is whether companies should profit from tax-exempt activity
).
-
"The Proposition 198/Gann Amendment prevents SB-562 from being implemented."
-
This is not addressed here. Discussion about this began this week at the Assembly Informational Hearing on Implementation Considerations for Universal Coverage February 5th.
-
This is not addressed here. Discussion about this began this week at the Assembly Informational Hearing on Implementation Considerations for Universal Coverage February 5th.
-
Legislative Course to Come
-
SB 562, which passed the Senate 23 to 14, would have to return to the Senate floor for another vote if it is amended in the Assembly with a funding plan and passes with a 2/3 vote.
-
After introduction, a bill goes to the rules committee of the house, which assigns it to the policy committee appropriate to the subject matter, for its first hearing. During the committee hearing, the author presents the bill to the committee, which may hear testimony in support of or opposition to the bill. The committee then votes on whether to pass the bill out of committee, or that it be passed as amended. The Fiscal committee reviews the bill since it has financial implications for the state. Bills may be amended several times. It takes a majority vote of the committee membership to pass a bill and send it to the next committee or to the floor.
- SB 562, which passed the Senate 23 to 14, would have to return to the Senate floor for another vote if amended with a funding plan. The house of origin may concur with the amendments by a 2/3 vote and send the bill to the governor or reject the amendments and submit it to a two-house conference committee. If either house rejects the conference report, a second (and even a third) conference committee can be formed. If both houses adopt the conference report, the bill is sent to the governor.
-
SB 562, which passed the Senate 23 to 14, would have to return to the Senate floor for another vote if it is amended in the Assembly with a funding plan and passes with a 2/3 vote.
back
back
-
Evidence Based Medicine has failed - which has corrupted Academic vs Clinical control systems, allowing Financial dominance
- Terminology has imprecise and misleading meaning ("Whopper" vs Hamburger). It is effectively Applied Epidemiologic
Statistics - Public Health processes.
-
Statistical Generalizations (
EBM
blurs information, sorts it in defined bins, pretend all in the bin are equivalent)
-
2x2 Contingency Table is a starting point - This is a Graphical Compartmentalization of Possibilities, but introduces significant errors depending on ones preferences (False Positive/Negative, True Positive/Negative inclusions or exclusions).
-
Null Hypothesis - black/white replaces red, yellow, blue, greens
- creates a yes/no (2 possibilities) from 2x2 table (4 possibilities), ignores cases to get a yes/no answer
-
always totally wrong in some individual cases - have to accept intrinsic error in knowing
-
Distribution replaces individual values
- Emphasizes groupings and averages.
- The individual becomes invisible
-
Shape of distribution is mostly ignored
-
Errors are invisible unless they combine to a pattern
- Bias of the Mean - extremes dominate the data, hide the middle and introduces error
- problem separating data from error
- errors average out or even dominate the data
- accumulation of errors (creates heterogeneity)
-
Contamination of data destroys significance
-
Overgeneralization - Standard Error of the Mean (
SEM
) problem (averaging averages)
-
Statistics (
description
of static known data) vs Probabilities (
prediction
of future outcomes)
-
Changes over time distorts age dependent data on individuals
-
Statistical, Medical, Clinical Significance are not interchangeable
-
Negative/Positive Predictive Value
- Medical Statistics: Averages Ratios vs Numbers - less theroretically
founded
- Less precise than standard Statistics, because a comparison of Rates, not Numbers.
- 1/2 + 1/2 does not equal 1/4 - the arithmetic of ratios is non-intuitive
- percent vs absolute differences in interpretation is important, often unreliable clinical indicators
- denominator dominates, not the event numerators.
-
p-values do not relate clinical significance
-
The vast majority of studies are done in research settings, by care delivery providers or by policy-reviewers, at a macro-level with published findings that are not prescriptive.
( 140-14 ) 140-14 How providers can lower costs 018896. pdf <<<OPEN
back
-
Electronic Health Records under-perform, increases overhead >20%, decreases patient load by 20%
-
Cumbersome work flows and ongoing training and maintenance costs are a problem.
- Evaluation of EHR
improvement in Outcomes
- Medical work is far from being a straightforward process. Rather, it is fundamentally a multitasking, cognitive, distributive, collaborative, interpretative, interruptive, responsive, and reactive procedure. The model of workflow in electonic
systems however tends to conceptualize order creation and communication in a predefined, linear, and stepwise fashion.
-
Use of Computer Medication Orders (
CPOE
) is a distinct process from Patient Clinical Charting by providers
-
CPOE
benefits
- Remote access to enter orders or view their status was highly appreciated
- A study calculated a 75% reduction in the number of verbal and telephone orders
-
Studies show that the rate of order countersignatures improve.
-
CPOE
Negative aspects
- Using CPOE
systems was found to be time-consuming for clinicians.
More time was spent on ordering. A personal comment is that the mental manipulation of data required is taxing and distinct from physician care.
- Using CPOE
systems was found to be time-consuming for clinicians.
More time was spent on ordering. A personal comment is that the mental manipulation of data required is taxing and distinct from physician care.
- The application of CPOE
systems changes teamwork in two ways: by re-delegating tasks between co-working providers, and by changing communication channels and collaboration mechanisms. The model of strict and physician-dominant authorization underlying CPOE
therefore may partly mismatch with the negotiated and co-constructed nature of ordering practice.
- A computerized laboratory order entry system shifts some responsibilities of the laboratory staff to the clinicians on the ward. Studies have shown that a literal translation of this formal and hierarchical authorization in CPOE
limits the effective contribution of all providers in the ordering activities. The ability of these systems to integrate different pieces of information and to communicate their contextual meaning is limited.
- In one study, the pharmacists reported that the system took away some of flexibilities
of their paper-based system to allow them to take clinically justified decisions in cases they disagreed with particular physician orders. Two studies mentioned a new responsibility for nurses to reconcile the orders OPEN by pharmacists with the physician-initiated orders.
In addition, nurses had to ensure that a verbal order had been entered by physicians, while this issue was not crucial before.
-
CPOE
benefits
- 92% of orders entered directly by MD’s, and >49% of all physician orders entered using standardized order sets
- CPOE computer order entry can decrease Medication turn around time and signature requests 23-92%.
- Most published studies have been performed at academic hospitals. Little is known about the effects of CPOE at community hospitals.
- No control group generally (ie, paper charts, staffing with RN's)
- How often does computer access to past comprehensive medical history, drug allergies, medications, laboratory improve results.
- Most important information network is the in the Physician and Nurses head.
-
Hospitals commit significant financial resources toward equipment, software, IT staff, and training.
-
A difference was also seen in high harm events where
0.5-0.6% of health IT-related events
resulted in permanent harm or death
compared to 0.9%-1.0% of events that did not involve health IT , although the number of cases was small.
- Medical work is far from being a straightforward process. Rather, it is fundamentally a multitasking, cognitive, distributive, collaborative, interpretative, interruptive, responsive, and reactive procedure. The model of workflow in electonic
systems however tends to conceptualize order creation and communication in a predefined, linear, and stepwise fashion.
-
Computerized Provider Order Data Entry (
CPOE
) Electronic Record Systems primer
( 116-01 ) 116-01 OpenClinical _ CPOE . pdf <<<OPEN
-
Big Data
( 101-01 ) 101-01 ei-evolving-role-data-decision-making HL.pdf
- BigData-driven decision making increases productivity +5% , but costs overhead -20% . (101-01)
- BigData is frequently used in finance decisions , which tends to be structured and predictable. (101-01)
- " Not everything comes in a nice record format”. (101-01)
- "Companies use the data to drive decisions more often across all parts of the organisation ." (101-01)
- "There is a fundamental skill missing in the big data and analytics world that has nothing to do with technology or data. That gap: knowing how to frame and articulate the question being asked in the first place ...if [companies] do not ask the right question, they will not find a meaningful answer. In many cases, they will just confirm their own biases ." (101-01)
- "The key in many instances is not so much technology as it is people qualified to use it. ... [E] ven if companies can find people who can handle the technical side of data analytics, these technical specialists often are unable to communicate their findings to the business." (101-01)
- "The government are very keen at amasing
statistics. They collect them, raise them to the nth power, take the cube root and prepare wonderful wonderful diagrams. But you must never forget that every one of theses figures comes in the first instance from the village watchman, who just puts down whe
he damn pleases."
-
"Computers, Electronic Data and the Vietnam War" - Donald Fisher Harrison 1994 (
23-0
)
-
"Computers, Electronic Data and the Vietnam War" - Donald Fisher Harrison 1994 (
23-0
)
back
- Corporate Health Care Profit Gains have been phenominal
since 1981, increasing at or more than GDP each year: 6 times the GDP increase from 1960 to 2013 (0.01 to 1.8) compared to (0.5 to 14).
(147-01 ) 147-01 CorpProftsGDPgraphic.pdf
back
back
-
Tying Health Care Funding to Taxation and Employment
-
There has been concerted efforts to monetize every type of asset that can be identified, or the laws changed to allow private profit from what are the shared commons. There is simple arithmetic at play for this in Health Care: there are 100 million Americans effectively working, and there are 300 million Americans that need the same healthcare. The numbers don't add up, and the more complicated the pay-backs and extortion-type skimming off the top there is, the harder it is to reward the hard work and responsibility it requires to care for a living creature (or maybe be a steward of inanimate natural resources).
-
There has been concerted efforts to monetize every type of asset that can be identified, or the laws changed to allow private profit from what are the shared commons. There is simple arithmetic at play for this in Health Care: there are 100 million Americans effectively working, and there are 300 million Americans that need the same healthcare. The numbers don't add up, and the more complicated the pay-backs and extortion-type skimming off the top there is, the harder it is to reward the hard work and responsibility it requires to care for a living creature (or maybe be a steward of inanimate natural resources).
-
ECONOMIC ENSLAVEMENT
( 118-03 ) 118-03 How Did Economists Get It So Wrong_ - The New York Times.pdf
-
Insanity is doing the same thing again and again and expecting a different result. The current situation in Health Care is reminiscent of the collapse if the hospitals in late 1990's. The basic economic driver was capitation, the idea that when you do less you get paid more. It is also reminiscent of subsidies to milk farmers, to dump their milk in an effort to maintain profit pricing. The key difference at this time can be seen in the structure of the ACO itself. Whereas the contracts of the Physicians hired by the Hospitals in the 90's had to be bought out at great cost, requiring the Federal Government to assume great debt in the process (still owed).
-
If you tour hospitals it becomes clear that work situations more and more resemble Luxury Hotels which hide oppressive medical factories, with burnout rates >50% for Doctors, and Nurses not far behind. Patients are wheeled from one section of the maze to another with little awareness what actually goes on in each cubby hole. In fact, as security has injected itself more and more, the locked corridors resemble prison complexes. (118-03)
-
The response of our Investor Model of Business is simply to get rid of Doctors and Nurses as they are made less efficient and more of a liability ("cut the fat"). However, replacing Physicians has required massive investment in new technologies and re-structuring of staffing such as using Hospitalists, which has proved to be more expensive. Massive subsidies funnel profits up to the control class, and has led to a spiraling financial collapse of these institutions to the bottom. More massive support will be required to maintain it. (118-03)
-
Medical businesses have morphed to focus on profit by finance rather than producing health.
Until
the Great Depression
, most economists clung to a vision of capitalism as a perfect or nearly perfect system. That vision wasn’t sustainable in the face of mass unemployment, but as memories of the Depression faded, economists fell back in love with the old, idealized vision of an economy in which rational individuals interact in perfect markets, this time gussied up with fancy equations (utilizing un-testable and dangerous statistical techniques such as Bayesian Analysis). They turn a blind eye to the limitations of human rationality that often lead to bubbles and busts; to the problems of institutions that run amok; to the imperfections of markets — especially financial markets — that can cause the economy’s operating system to undergo sudden, unpredictable crashes; and to the dangers created when regulators don’t believe in regulation.
(118-03)
-
The self-deception required; the mantra that the taskmasters are infallible; the idea that if only the worker bees would follow "the protocols"; all lead inevitably to gross abuses and predictable failure. In many ways we have a Medical Economic Bubble that is bursting. CFO's and non-physician Administrators pretend to herd the necessary functions of the system, even without being physically present on site. (Employees at the level of Department and above are almost never in-house from 6pm through 6am. They get their information mainly thru electronic system reports, and administrative meetings during the day. These exclude any of the actual involved parties who are sleeping, and rely on the grape-vine system of gossip to make decisions. When micromanaging control is anonymous, accountability becomes a farce. And there is great economic overhead to this system which is bankrupting the Hospitals once again. (118-03)
-
At dire economic times economists may turn to the insights of John Maynard Keynes. Keynes did not, despite what you may have heard, want the government to run the economy. He called for active government intervention — printing more money and, if necessary, spending heavily on public works - to fight unemployment only during slumps
. Keynes considered it a very bad idea to let markets where speculators spent their time chasing one another’s tails dictate important business decisions: “When the capital development of a country becomes a byproduct of the activities of a casino, the job is likely to be ill-done.” Those who profit by concealing and shifting speculative risk convince others that it is not a problem.
(118-03)
-
By the 1980s, finance economists, notably Michael Jensen of the Harvard Business School, were arguing that because financial markets always get prices right, the best thing corporate chieftains can do, not just for themselves but for the sake of the economy, is to maximize their stock prices. The theoretical model that finance economists developed assume that every investor rationally balances risk against reward — the so-called Capital Asset Pricing Model, or CAPM (pronounced cap-em) — is wonderfully elegant. And if you accept its premises it’s also extremely useful. CAPM not only tells you how to choose your portfolio — even more important from the financial industry’s point of view, it tells you how to put a price on financial
derivatives
, claims on claims. Medicine has been enveloped with Investor Capitalism. The computer printouts provide proof how it is working until...
(118-03)
-
We rarely ask the seemingly obvious (though not easily answered) question of whether asset prices make sense given real-world fundamentals like earnings (productivity). Instead, we ask only whether asset prices make sense given other asset prices (cutting up the pie.) We do not factor in diminishing returns from the cost-cutting (the only tool large corporate executives have to balance their books, since they produce no product other than control of other's production), as final profit ignores just where the profit is generated. Since the profits require projecting assets and liabilities into the future to determine current profit, accounting systems fail to provide the necessary transparency. One market segment gaining at the expense of another cannot be distinguished from profit from productivity.
All the signs are there for a collapse of the Hospitals as seen in the late 1990's which required massive Government bailout and the assumption of debt. The Executive Class reaps all the benefits. Others bear all the burden. (118-03)
- SB-562 actually does not
let government run the Medical Economy
. It does takes steps to remove some very ineffective parts of the process (such as private health insurance, restriction of access to care, and forced un-productive administrative technologies) which are needed only to support the pricing structure from collapsing. SB-561, like Medicare, runs no hospitals, offices or operating rooms. In our common discussions we have conflated Payroll Taxation and Employer Provision of insurance, with the actual Provision of Care, as if it is only what premium you have to pay every month that matters. (118-03)
-
Insanity is doing the same thing again and again and expecting a different result. The current situation in Health Care is reminiscent of the collapse if the hospitals in late 1990's. The basic economic driver was capitation, the idea that when you do less you get paid more. It is also reminiscent of subsidies to milk farmers, to dump their milk in an effort to maintain profit pricing. The key difference at this time can be seen in the structure of the ACO itself. Whereas the contracts of the Physicians hired by the Hospitals in the 90's had to be bought out at great cost, requiring the Federal Government to assume great debt in the process (still owed).
-
SLAVERY
( 118-01 ) 118-01 Did slavery make economic sense_ - Economic history.pdf
( 118-02 ) 118-02 economy - Was slavery economically most efficient system in the ancient_agricultural era_ - History Stack Exchange.pdf
-
Slavery is an efficient form of labor from the view of Net Profit (prevents marginal benefits from going to workers, keeping the Worker Class separate from the Elite Class and limiting social mobility.) Basic Economics teaches that wealth comes from the excess capacity beyond subsistence. Slave workers are excluded from wealth (all goes to the top 1/10th of 1%). The ultimate result of increased efficiency can be a type of economic slavery, with eventual diminishing returns. The following is stolen freely from analysis papers. (
118-01
)
-
In agriculture, slavery is the most efficient system for a manorial system
, even though it is less efficient compared to free labor farming on small farms for example. Paid, freely negotiaing
workers fall somewhere in between. (Tenant farmers and serfs, not totally slaves, are less efficient.) In other words, people must own their land and own what they produce to be productive or they are disincentivized
. And depressing labor wages creates a labor force that although appearing to have a choice, practically do not. (
118-01
)
-
Slaves are made productive through violence
. This also doesn't work on a feudal serf who is the responsibility of the manor. The proof for this idea comes from the numerous emancipations of serfs or slaves throughout history. Agricultural production will fall by nearly half in the first few years as a result of the upheaval but will soon recover and greatly overtake the past production levels if land ownership
is implemented. (
118-01
)
- In civilizations where land is the measure of wealth, there is a tendency for the wealthy to buy up all the land
. When Rome started winning many wars, there was a greater and greater gap between rich and poor
. The rich were able to establish a plantation system. Therefore, even before industrialization, slavery was less efficient. The elite attempt to make it just efficient enough for them to have plantations. (
118-01
)
-
It can be argued that slavery is always less efficient than freedom, and any man will produce more when working for his own interests rather than a masters. Does this not apply to a corporate system that constricts worker benefit with all gains going to shareholder profit?
(
118-02
)
-
A newer form of enslavement - workers
forced to be less productive
under the legal and illegal power of corporate collectives, is often through violence, threat of violence, or judicial violence (losing a home because of a minor payment failure). This also fits nicely into a stock options approach to compensation. (
118-01
)
-
This Debt Slavery is economically inefficient compared to free labor (no profit tax on producers). In the American colonies, the consistently poor were sold into slavery to the lowest bidder for short periods of time of a year to five years, prior to the invention of poor houses. There was limited charity and government aid, but some people needed long term assistance. It was a consistent problem that these slaves would not be able to bring enough income for the master and thus were often very poorly treated, not given enough food and basic clothing. (
118-01
)
-
Historical intention was to improve the lot of the poor person who was likely begging for food in the street, but the system obviously failed. It makes a bit of sense that those who are poor have low earning potential, since many would be elderly or suffer from disabilities. For what its worth, the Romans actually did ban debt slavery. Broadly allowing enslavement has documented negative economic effects, such as increasing parasitic lending practices and bad business investments. (
118-01
)
-
Alfred Conrad and John Meyer in more recent analysis calculated the rate of return on investing in slaves. They reckoned that “slave capital” earned at least equal returns to those from other forms of capital investment—such as railroad bonds. The rate of return on slaves could be as high as 13%—compared to a yield of 6-8% on the railroads. (
118-01
)
- There was also a big industry in slave finance, procurement and transport. And by the end of the 17th century, there were about 70,000 slaves transported each year. And some financiers became fabulously wealthy. Christopher Codrington
made a lot of money from the sugar trade, and made large bequests to All Souls College, Oxford. (
118-01
)
-
Slavery is an efficient form of labor from the view of Net Profit (prevents marginal benefits from going to workers, keeping the Worker Class separate from the Elite Class and limiting social mobility.) Basic Economics teaches that wealth comes from the excess capacity beyond subsistence. Slave workers are excluded from wealth (all goes to the top 1/10th of 1%). The ultimate result of increased efficiency can be a type of economic slavery, with eventual diminishing returns. The following is stolen freely from analysis papers. (
118-01
)
back
- (
15-0)
Pollin-Economic-Analysis-SB
-562 HLa.pdf
- (13-01) AHPI _STUDY_Cost_Per_Covered_Life HL.pdf
- (23-H ) Single_Payer_Implications_Employer_Sponsored_Care HL.pdf
- (183-01) The Social Transformation of American Medicine, by Paul Starr (1983, 2017)
- ( 24-01 ) (Medicare Is Not “Bankrupt” _ Center on Budget and Policy Priorities.pdf)
- (135-0) Rosemary Gibson References
- Books by Rosemary Gibson:
- Online Video: The Battle Over HealthCare
Highlights (Minute Mark into Video) w- Overuse - (48.25-49.28)
- End of life care, Overuse expectation - (55-59)
- Cost of Education - (1.01.30-1.04.30)
- Cost of Medical Care, Waste - (59.10-101)
- What can you do, 30% Waste - (34.26-35.30)
- GI, primary care overload, lawsuits, toxic bubbles, made medicine political
- (49.30-55)
back
back
The CA State Assembly this week held the 5th and 6th Informational Meetings of the Select Committee, the "Assembly Informational Hearing on Options for Universal Coverage" (non-legislative). It was the first meetings where SB-562 itself was discussed at all. Dr. Pollin from the University of Massachussetts testified on Wednesday. He authored the Report* evaluating SB-562 in May 2017 sponsored by the California Nurses Association. The presentations (2/5 2pm, 2/7 10am) can be viewed in Archive at the State website: http://www.calchannel.com/. Clic on the bars to the top left and scroll to those dates to view. CNA has been given 30 minutes of testimony time so far, and report having 17 amendments for SB-562 to address the funding mechanism. Although it is 10 hours of testimony, these give an overview where we are in legislative, political and administrative processes.
Expert testimony given in response to Select Committee Congressman Wood's questioning (Scott Graves of the CA Budget and Policy Center on 2/5, at Hour 3 Minute 26) indicated that if the Legislature takes on the task of evaluating and completing SB-562/2.3 with the proper Assembly Committee actions, the task could be accomplished in "a matter of months" (which requires 2/3 vote of both Houses). If it is done by outside Groups taking on the task, he estimated it will take "1+ years" (which requires 50% approval by the Voters through a Constitutional Proposition).
What we have learned in researching this report and since is that Health Care can not be party or political. Health Care is, when examined, not a good Campaign Issue. Just corner any Politician marketing "Me-Too Universal Access" or running away from CSP/2.3, or those who lose donors and elections even daring to speak about it. For over 100 years, evaluations have echoed again and again that Single Payer is the way to control Health Care Costs for America, while providing, as demonstrated in the rest of the world, Universal Appropriate Care. Since management of Care already regulates at the State level, it makes the most sense to fund it there. If we look a little deeper into the information some have told us is "too overwhelming to bother", we will make it work. We provide this Workbook to help in that task.